What is the Infection Rate of COVID-19 in Dental Offices?
Article Link: https://jada.ada.org/article/S0002-8177(21)00658-9/
The Covid-19 pandemic has had significant impacts on many aspects of society. While we are still elucidating the short and long term effects of the virus, studies are coming out that are starting to unravel these effects. Once such study explores the incidence rate of Covid-19 amongst practicing Canadian dentists to determine exposure rates in a dental setting.
There is evidence indicating that healthcare providers have an increased risk of covid-19 infection as compared to the general population. This also makes sense as healthcare workers are those who are directly treating, and therefore exposed to, patients with active covid-19 infections. This is especially true of dentists, who work in the oral cavity with aerosolizing techniques which aids in transmission of the coronavirus.
Dentists, which are a high-risk group of healthcare providers, were not identified as a group in these previous studies. However there is some data showing a confirmed or probable case of covid-19 infection due to the line of work that ranges anywhere from 0.9% to 2.6% from dentists in the US.
This study found results that 1.08% of dentists were covid-19 positive between July 29, 2020 through February 12, 2021. This rate was lower than the infection rate of the general population, which has a number of interacting factors which include:
- Pre-screening of patients.
- Rigorous infection control protocols.
- Physical distancing.
- Appropriate mask quality and techniques.
- Personal protective equipment (PPE).
While the study believes that the vaccination could play a role, there was more than 4 months prior to the availability of the vaccine. Additionally, while the study took saliva samples, the authors understood that while nasopharyngeal swabs are the best screening method, the impracticality eliminated it as a feasible data collection method.
The conclusion is that the infection rate amongst dentists is very low. This is reassuring for those who have missed their regular dental visits due to fears of Covid-19. When following enhanced infection control protocols, going to your dentist is safe. If you have further concerns, call your dental office and ask about their protocols so you can receive the care you need.
How Does Diet and Fluoride Affect Cavities in Children?
Article Link: https://www.mdpi.com/2304-6767/10/6/96
The relationship between consumption of sugar and health has been a concern of health care professionals for many years. As it relates to dental health, it is generally accepted that processed sugary foods and drinks increase the risk of dental caries as well as periodontal disease. In Latvia, tea drinking is considered historical and cultural. Sugar is often added to tea, approximately 4.7 – 7.3 teaspoons daily amongst children in Latvia. This has led to a high prevalence and severity of dental caries amongst children.
This study investigated the effects of fluoride varnish and oral hygiene instructions affected cavity rates over a three year period for 6 year olds and 12 year olds in Latvia. The children were split into those who got fluoride varnish and those who did not, in two age groups of 6 and 12 years of age. Everyone received the same hygiene instructions and those who got the fluoride varnish received it every 3 months.
Cavity rate was evaluated using the decayed, missing, and filled teeth/surfaces (DMFS) which is the predominant method to evaluate oral health. It refers to the amount of teeth that are decayed, missing, or filled which indicates the status and amount of disease, both past and present. Simply put, the higher the DMFS, the more susceptible, either past or present, the patient is to dental caries.
The researchers found that despite challenging dietary habits, that a quarterly application of fluoride varnish decreased the prevalence of caries. This furthers the evidence that fluoride treatment is the treatment of choice to remineralize cavities to keep teeth healthy.
Interventions to Improve the Oral Hygiene of Individuals with Alzheimer’s Disease: A Systematic Review
Article Link: https://www.mdpi.com/2304-6767/10/5/92
Alzheimer’s disease causes the afflicted to maintain many activities of daily living (ADLs) due to the neurodegenerative process. This includes hygiene habits such as teeth brushing, flossing, and visits to the dentist. Patients may even display behavior changes which compounds the difficulty in proper hygiene.
This study investigated the methods of oral hygiene, including the usage of manual or electric brushes, flossing, mouthrinses, professional cleanings, oral hygiene instructions and/or training, and whether or not regularly scheduled dental visits were made. The authors found that there was an improvement on the plaque index of the patients who had some type of intervention. They also found that there are population groups that are more susceptible to adverse outcomes, in particular low and middle income countries with poorly developed long term care systems. It was also found that the nature of the disease impaired not only oral health but the ability for dental services. This means that the interventions given may not have been equally applied to the Alzheimer patients.
The authors concluded that there was a very large lack of published studies available for the use of oral health interventions among patients afflicted with Alzheimer’s disease. Although they were able to find some data supporting the use of interventions, they stated that the studies were of institutionalized patients with small sample sizes and did not account for the severity of the disease. With more data, better comprehensive strategies can be implemented based on the patient’s stage of the disease to get the best outcomes.
Implant-Retained Mandibular Overdentures: Patient-Related Outcome Measurements after Seven Years of Function
Article Link: https://www.mdpi.com/2304-6767/10/5/88
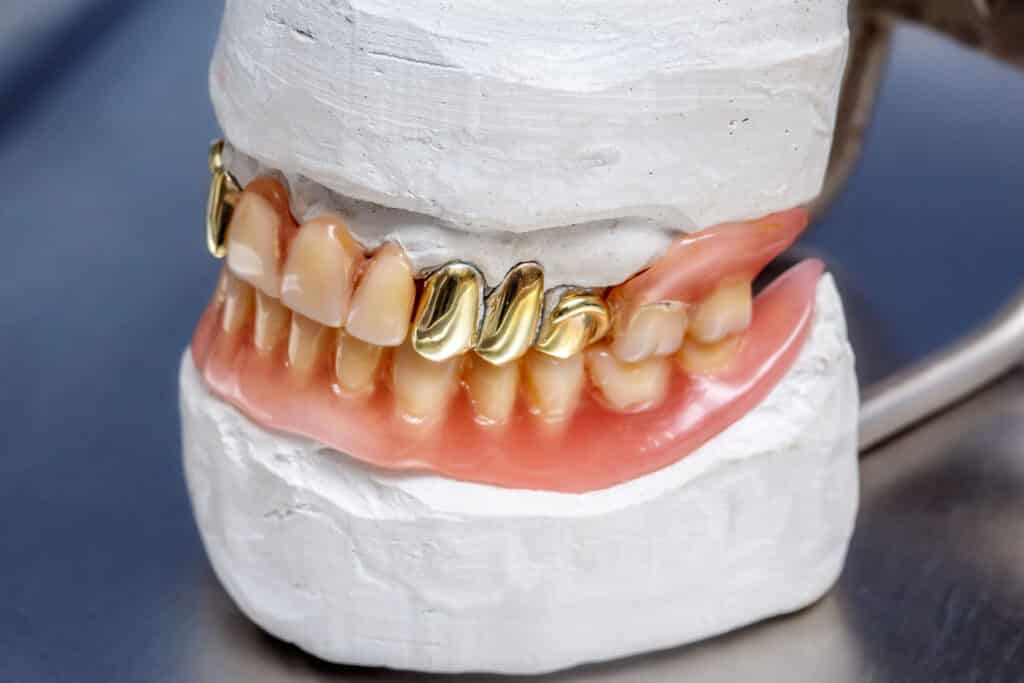
Those who have needed to have all their teeth extracted have what’s called an edentulous (without teeth) mouth that necessitates the usage of some type of prosthesis. Most commonly used are dentures. However one of the most common problems with dentures is the lack of retention and stability. This is due to the inherent nature of complete dentures – without implants, there is nothing to anchor the prosthesis to the jaw to provide stability and keep the dentures in.
With the addition of implants to keep the dentures in place, patient outcomes are greatly improved. This study aimed to follow two different attachment types of implant retained overdentures on the mandible over seven years. The two different styles are a ball or a locator attachment.
The authors found a very high survival rate of 98.7% of all implants. They found that of the total 438 maintenance visits, the locator style has almost 3 times the number of visits at 121 ball attachment vs 317 locator attachment maintenance visits. 78% of the total maintenance visits for both styles were easily solved chairside. The costs to maintain both styles over the 7 years was minimal and amount to less than 20% of the original treatment cost regardless of the style of retention.
In conclusion, the authors found that both styles of retention are a viable option and that the maintenance and repair costs are minimal. One aspect they authors did not mention is the type of material the locator inserts were made of. Traditionally they are made of a nylon material, which typically requires replacement up to a few times a year. However there are other materials such as the Novaloc system which typically requires less maintenance.
Was this post helpful?
Table of Contents
- What is the Infection Rate of COVID-19 in Dental Offices?
- How Does Diet and Fluoride Affect Cavities in Children?
- Interventions to Improve the Oral Hygiene of Individuals with Alzheimer’s Disease: A Systematic Review
- Implant-Retained Mandibular Overdentures: Patient-Related Outcome Measurements after Seven Years of Function