Many people have needed to extract one or more teeth for various reasons. While some fear of a tooth extraction is warranted, most surgical extraction procedures are straightforward. Getting a tooth pulled can be due to many reasons, however the most common are tooth decay, a tooth infection, advanced gum disease, and a severely fractured or damaged tooth. The extraction procedure may be completed by general dentists, an oral surgeon, or other specialist. This will depend on the type and complexity of the tooth extraction.
What are Dental Extractions?
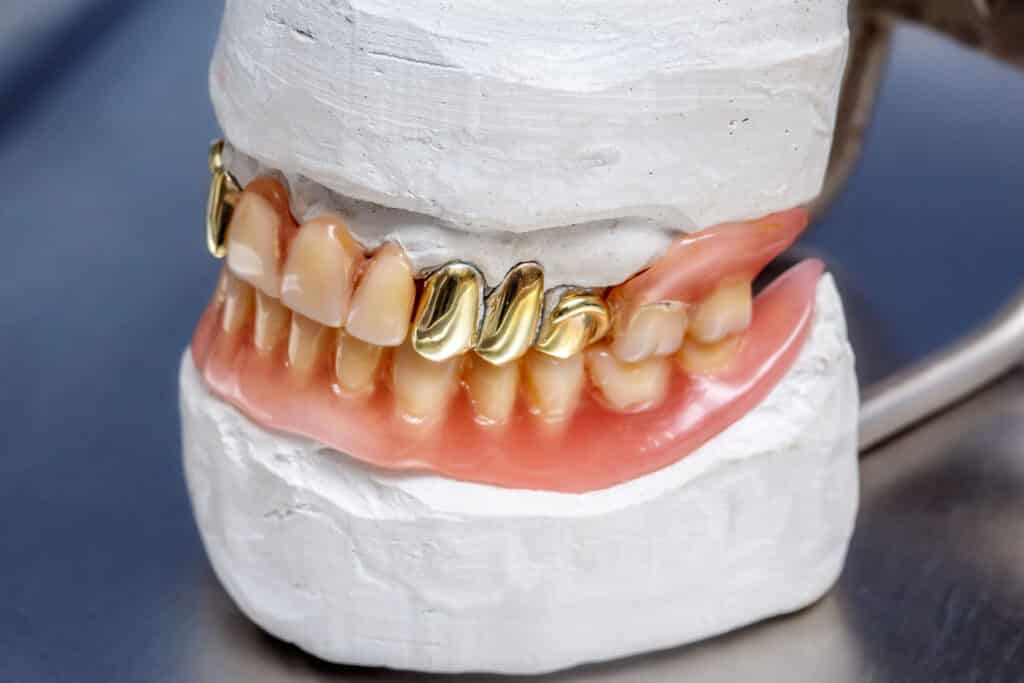
According to the American Dental Association, dental extractions are the removal of teeth. While each dental extraction is considered a surgical procedure, most are categorized as either a simple dental extraction or a surgical dental extraction. After the affected tooth is removed, the tooth may be replaced with a dental implant, fixed partial dental or dental bridge, or a removable prosthesisAn artificial body part, which is often lost due to disease or trauma. such as a partial or full denture.
However not every tooth extraction required replacement of the missing tooth. For instance wisdom teeth are not required to live a normal life. Other tooth extractions may be completed for crowding or orthodontic reasons as well. Many people are able to live a happy and fulfilled life if they have enough remaining teeth.
When Do I Need a Dental Extraction?
Most often a tooth extraction is needed due to an infection, severe pain, advanced tooth decay, trauma, advanced gum disease, crowded teeth, or prophylactically. While some tooth extractions are completed on asymptomatic teeth, many are done due to a dental emergency.
Dental Infection
Infections can affect many places in the mouth such as the gum tissue or the jaw bone itself. The primary risk is that harmful bacteria can travel throughout the entire body and can affect not only other teeth but also critical organs such as the heart. A tooth extraction is often the fastest and easiest solution in order to improve oral health.
Severe Pain
Dental pain can debilitate even those with a high pain tolerance. When a tooth is causing so much pain that you cannot sleep or function normally, dental treatment is required. While a tooth extraction is the fastest solution, removing a tooth that could otherwise be saved may not be the best long term solution.
Trauma
Sometimes unpredictable, acute trauma can render a tooth non-viable. When damaged in this way, the tooth can break in many ways, including right at the gum line, under the bone, or even avulse right out of the tooth socket. If there is not enough remaining structure to save it, a tooth extraction may be in order.
Advanced Periodontal Disease
If the gum tissue surrounding the natural teeth are diseased, the teeth can become loose enough to require a tooth extraction. This typically occurs in those who are susceptible to gum disease and/or do not get regular professional cleanings.
Crowded Teeth
Small, underdeveloped jaws may result in not enough space. When this is the case, select teeth are removed to give more space for the other teeth. Most often premolar or bicuspids are removed then orthodontics or braces straightens out the remaining teeth.
Prophylactic Tooth Extraction
Teeth are also removed to prevent common diseases or problems. Third molars, or wisdom teeth, are the most common instance of this. Often due to lack of space, improper eruption, or difficulty keeping clean, wisdom teeth are removed. Sometimes it is a single tooth extracted, but often multiple tooth extractions are done to reduce the number of surgeries especially if general anesthesia is required.
What Tools are Used for Dental Extractions?
While the instruments or dental tools used to perform tooth extractions may appear archaic, they are all designed to serve a specific purpose. The goal is for an atraumatic tooth extraction which results in reduced surgical site pain and discomfort. In other words when a tooth extraction is rendered without excessive trauma to adjacent gum tissue and bone tissue, there is less pain immediately and hours after the extraction.
Elevators or Luxators
Used in almost every tooth extraction, the instrument called elevators and luxators have a small curved tip with a handle. The main purpose is to place the tip ideally between the tooth and bone tissue. Then steady pressure is applied to push the tooth against the surrounding bone which expands the tooth socket. This will loosen the tooth enough to be removed with forceps.
Dental Forceps
There are many types of forceps, each with a different working end that clamps around the tooth. Pressure is again applied to expand the jaw bone immediately surrounding the tooth. Once loose enough, the tooth is removed while a clot forms in the extraction site.
What are the Most Common Extractions?
When getting a tooth pulled, the most common classifications are a simple extraction, surgical tooth extractions, and varying types of impacted extractions. Common scenarios include emergency extractions and wisdom teeth extractions.
Simple Tooth Extraction
This basic oral surgery may or may not manipulate the soft tissues around the tooth to be pulled. However there is no use of a handpiece to section the tooth or remove bone. Typically the tooth pulled is numbed with local anesthetic and removed in one piece.
Surgical Tooth Extraction
While very similar to a simple tooth extraction, the surgical component refers to when a handpiece is used. The affected tooth is split into multiple pieces or bone is removed. This is often done when there is not enough tooth structure for a simple tooth extraction.
Impacted Tooth Extraction
Impacted teeth refers to teeth that are either partially or fully covered by hard or soft tissues. Wisdom teeth are the teeth that are most often impacted. This type of maxillofacial surgery requires accessing the teeth by reflecting the gum tissues and sometimes also removing bone. Then to remove teeth, the process is essentially the same as the other types of dental extractions. Sutures are then placed in a way to promote healing and recovery.
What Can I Expect During a Dental Extraction?
If only local anesthesia is used without moderate sedation, what is mostly felt is pressure and jarring noises. Once anesthetized, there should be no sharp pain. If there is any, let your general dentist or oral surgeon know and they will get you comfortable.
After proper diagnosis, discussion of the treatment option and alternatives, and consents are completed, this is what happens during treatment:
- (Optional) Some form of sedation is used, whether it be nitrous oxideAlso known as laughing gas, is the chemical compound N20 that has many uses. In medicine, it is an analgesic and anesthetic. It is paired with oxygen when delivered in a dental setting., a pharmacological agent administered orally or intravenously or a combination of both.
- Local anesthesia is administered.
- Local anesthetics will prevent pain, however it will not prevent the sensation of pressure during the procedure. There will be a lot of pressure placed onto the tooth and jaw but it should not hurt.
- The periodontal ligament [PDL] is severed circumferentially around the tooth.
This is typically where the steps may vary depending on the type of extraction and how much of the clinical crown remains.
- An instrument is used to elevate or luxate the tooth against the alveolar bone. With enough elevation, the tooth becomes mobile.
- If part of the tooth breaks/fractures and there is no good purchase point, a surgical handpiece is used to either remove hard tissue or section the tooth into pieces.
- Sometimes a flap will be required to visualize the bone and tooth better. If this is required, typically a full thickness mucoperiosteal (FTMP) is completed.
- A set of forceps are used to grab onto the tooth and the surrounding bone is expanded even further until the tooth can be lifted out of the jawbone.
- Once all of the tooth is removed, the extraction site is visually inspected, debrided and irrigated. Additionally infected gums are removed.
- If necessary, sharp projections of the alveolar bone is smoothed.
- If bone grafting is required, it is completed at this time. The blood mixed with the grafting material may promote healing and immediate blood clot formation. This particular type of a graft, called a ridge preservation, is completed right after an extraction and may require a membrane.
The graft may be completed with various types of grafting material, sometimes even using platelet rich fibrin (PRF). PRF promotes healing in the extraction site and can improve oral health. - If a blood clot isn’t forming, materials or pressure is applied to reduce bleeding. The soft tissue is approximated and sutures are placed, tacking down a membrane if one was used.
- Hemostasis is verified at this stage. If moderate or general anesthesia is used, the patient then recovers and is eventually dismissed.
All in all, the primary feeling will be that of pressure, however there shouldn’t be any sharp pain. Popping, cracking and crunching sounds are all normal but can be unpleasant. Ear plugs or noise canceling headphones can be helpful, but the sounds may not be completely nullified, especially when extracting maxillary teeth. Speak with your local dental office if you wish to explore sedation for any extractions.
Why Do Dental Extractions Hurt?
While not as invasive as open heart surgery, dental surgeries are still a surgery. Anesthesia is administered, tissue is manipulated and aggravated in the process of all extractions. The surgery will elicit an inflammatory response and in addition to the purposeful trauma of surgery, these result in pain at the extraction site. Even atraumatic surgeries will result in some post operative discomfort, although smooth surgeries typically do not cause as much discomfort as complicated ones.
This is not to say that all dental extractions are painful. A simple extraction done atraumatically with proper post operative handling can be painless after the extraction. The type of surgery, difficulty, post op care, age and health of the patient all play a role in the overall postoperative discomfort.
What are the Most Common Complications of Dental Extractions?
There are many complications that occur after any dental surgery. We’ll categorize the complications into minor and major: minor occurs with almost every surgery but require no intervention while major are much less common but may require some intervention. Listening to what your dentist tells you will let you know what symptoms are normal and which ones aren’t.
Minor Complications
It is normal and expected to experience the following after dental extractions:
- Pain
- Swelling
- Redness
- Hyperalgesia – A painful response to normally non painful stimuli. For example, a minor cut hurts upon gentle palpation whereas the same stimuli does not hurt on healthy skin.
- Soreness
- Blood tinged saliva – The blood clot is exposed to saliva and may result in slightly red saliva but this is considered normal.
- Food impactionWhen food gets stuck in between teeth. This causes irritation in the gums and can be very uncomfortable. until the gums completely heal and smooth over.
These are all normal for hours after the extraction and do not require any intervention, with the exception of excessive pain. The main goal of pain management is not to completely eliminate pain but rather to make the pain level manageable. As inflammation and pain peaks after a few days, managing the pain until the mouth naturally feels better is the primary goal of postoperative analgesics.
Major Complications
These complications are not expected and the goal is always to avoid these.
Alveolar Osteitis (Dry Socket)
When a tooth is extracted, there is a hole that remains in the jaw at the extraction site. A blood clot will form in this space right after the tooth is removed, however the blood clot can be easily dislodged. If it is removed accidentally, it will expose the bone to the oral cavity and can be extremely painful.
Nerve Paresthesia
There is a chance that when teeth are removed that nearby nerves can get damaged, leading to temporary or even permanent numbness. This most often occurs from mandibular 3rd molar extractions. Luckily most of the damage to the nerve regenerates within 6 to 12 months.
Post Operative Infection
Due to there being exposed tissues intraorally as well as active bacteria in the mouth, there is a chance of an infection after dental extractions.
Fractured Root Tips
The variance in root anatomy means there will be long and thin roots that are easily prone to fracture. When elevating out teeth, teeth may fracture and root tips may be difficult to retrieve without damaging any surrounding tissues. It is safe to leave root tips if they are small enough if the surgeon believes he/she will cause more harm when trying to retrieve the root tip. Over time, the body will either sequester the root tip with no issues or it may become pathologic and require removal.
Damage to Adjacent Structures
Damage to nerves is the more common risk, however nearby structure may get damaged as well. An example is a root tip being pushed into the maxillary sinus which may require retrieval.
What Should I Do After an Extraction?
While most offices will give specific written instructions for what to do after any oral and maxillofacial surgery, here are some general tips for postoperative instructions. Always follow the advice of your dental office to ensure predictable healing.
- Avoid any actions which increase intraoral pressure and increase the risk of a dry socket. The following are a few examples:
- Using a straw
- Spitting
- Holding in a sneeze, as opposed to letting it go
- Playing wind instruments
- Do not smoke. This includes marijuana, cigars, vaping and of course cigarettes. While there is little conclusive evidence of the effects of marijuana and vaping, it is safer to assume the effects are detrimental to postoperative healing.
- Avoid strenuous activities. This includes all forms of exercise except for casual walking on a flat surface. This is to prevent any increases in intravascular pressure which can also lead to a dry socket. It is better to be a couch potato for a few days to avoid complications. I have even had a patient get a dry socket after lifting up her 3 year old granddaughter.
- Light duty when returning to work. While it may not be possible or practical to take time off work, it is a good idea to take up to a few days off work depending on the extensiveness of the surgery. When returning to work, ensure that it is light duty for a short time to avoid complications. You may need to ask your dental office to write a doctor’s note indicating specifics as it will vary from provider to provider.
- Use the pain medication as prescribed and do not combine any prescription medications with over the counter medication without approval from your dentist.
- Avoid the use of alcohol.
- Use cold packs to help reduce inflammation.
- Eat soft foods and if possible avoid chewing near the site of the surgery.
- Ensure you have a way to get in contact with your dental provider should a complication arise.
What Should I Do in Case of an Emergency After a Dental Extraction?
While it depends on what the emergency is, the best course of action is to first call your dentist to seek advice. Luckily, almost every emergency is preventable by following the given post operative instructions. However, complications do occur after surgery. Here are a few common complications and how to address them.
- Bleeding: While it is expected to have blood tinged saliva, a steady ooze from the socket site is not normal. Those taking anticoagulant medications are at higher risk. The first step is to get a clean damp paper towel or cloth and clamp down with moderate pressure for up to 30 minutes. This is the first step and will usually take care of any excessive bleeding. If it does not, contact your dental office while continuing to put pressure on the extraction site.
- Debilitating pain: It is expected to have some amount of pain and discomfort after an extraction, however if the prescribed pain regimen is unable to dull the pain to manageable levels, contact your dental office. The pain may require different medication or it may be due to a dry socket, both of which require professional intervention.
- Alveolar osteitis: Also known as a dry socket, this typically manifests as extreme pain that cannot be managed with medication. This requires anesthetizing the area, cleaning and debriding the socket, and either placing medicament to ease the pain or to reintroduce and stabilize another clot. Either way requires professional and immediate help.
- Abnormal swelling. This may be an indication of an infection. As a general rule of thumb, minor swelling is normal, however excessive swelling that causes facialThe ‘outside’ surface of the teeth that directly face either the lips or cheeks. asymmetry may be something more serious. If you are unsure, contact your dental provider and they will be able to give you further advice.
The majority of dental extractions heal without serious complications when the proper postoperative instructions are followed. If you are unsure whether or not you have an actual emergency, call your dentist and they will be able to guide you further.
What Do I Replace the Missing Space With?
There are generally 3 options to replace missing teeth: dental implants, dental bridges, or some type of denture. There is also the option of no treatment and to not replace the missing tooth. While implants are the gold standard to treat edentulismMissing some or all teeth in an area of the jaw., keep in mind it may not be the right option for you. For instance someone wanting to avoid all surgeries at all costs may choose a bridge or partial denture. There are extensive pros and cons to each option which we will briefly discuss. For more information, go to the corresponding page to make an informed decision.
Dental Implants
Pros
- Functions closest to natural dentition.
- Best esthetics.
- Shown so far to have the best longevity.
- Hygiene is similar to natural dentition.
- Considered the gold standard to replace missing teeth.
Cons
- Can be the most costly option.
- Requires surgery.
- May require an additional bone grafting surgery if insufficient bone exists to place an implant.
- Takes the most time due to healing requirements.
Dental Bridge
Pros
- Functions very similarly to natural dentition.
- Quicker turnaround time.
- Does not require additional surgeries.
Cons
- Cost can be similar to implants.
- Fair esthetics.
- Requires placing crowns on teeth adjacent to the missing tooth/teeth.
- Harder to clean, as floss must be threaded underneath the bridge.
- If recurrent cariesDental caries that reoccurs at the margin of an existing restoration. occurs, the entire bridge would likely need to be replaced.
Dentures
Pros
- Can be the most cost effective option.
- Able to replace the most number of teeth at a time.
- Does not require additional surgeries (with the exception of implant supported dentures.)
Cons
- Poor function, with significantly more difficulty in eating.
- Poor esthetics as compared to the other options.
- Can have poor retention.
- Can affect speech.
- Must be removed and cleaned multiple times a day.
- May fracture or be lost.
- Can be uncomfortable.
- The plastic teeth wear down faster than the alternative options.
Was this post helpful?
Table of Contents
- What are Dental Extractions?
- When Do I Need a Dental Extraction?
- What Tools are Used for Dental Extractions?
- What are the Most Common Extractions?
- What Can I Expect During a Dental Extraction?
- Why Do Dental Extractions Hurt?
- What are the Most Common Complications of Dental Extractions?
- What Should I Do After an Extraction?
- What Should I Do in Case of an Emergency After a Dental Extraction?
- What Do I Replace the Missing Space With?