A simple way to think about oral surgery is any procedure that involves the manipulation, removal, or addition of tissue within the head and neck. Most often people think the surgeries are limited to within the mouth, however it may involve the mouth, a single jaw, both jaws, the neck, the face or even the throat. Most oral surgery is completed within the oral cavity by either a general dentist or by various specialists.
When more advanced procedures such as corrective jaw surgery or corrective a cleft lip is required, oral and maxillofacial surgeons are going to be the doctor of choice. This is because this specialty focuses on reconstructive surgery and are trained and equipped to handle such an invasive, but life changing surgery. The simpler surgeries are often completed under local anesthesia with the occasional light sedation such as nitrous oxideAlso known as laughing gas, is the chemical compound N20 that has many uses. In medicine, it is an analgesic and anesthetic. It is paired with oxygen when delivered in a dental setting., while complicated procedures requiring general anesthesia will need to be completed in a hospital.
Dental oral surgery is commonly rendered to ensure or restore optimal oral health. There are a multitude of conditions and pathologies that require some type of oral surgery. The types of procedures that can be classified as oral surgery will include many types of procedures that range from a simple tooth removal to major orthognathic surgery, head and neck surgery and even some plastic surgery. Oral surgery can even include the procedure of a gum graft or treatments of advanced gum disease.
Who Can Perform Oral Surgery?
While many surgeries within the mouth are completed by a board certified oral and maxillofacial surgeon, there are other providers that perform various surgeries. For instance a periodontist, a dentist who specializes in the management of the bone and soft tissues of the mouth, can also perform many types of surgical procedures as well. Other dental specialists who regularly perform oral surgery includes endodontists (the specialty of root canals), pedodontists (the specialty of dentistry for children), and of course oral and maxillofacial surgeons who specialize in oral surgery. Of course, a general dentist is capable of rendering surgical treatment as well. In fact there are dentists who are experienced enough in some dental services that they limit their practice to a surgical practice only.

Which Dental Specialist Should I See?
The specific specialist will depend on the needs and goals of the patient. Minor oral surgery may not require an oral surgeon to be successfully treated. However the more complicated and invasive the procedure becomes, the higher the likelihood an oral surgeon would need to be seen. Wisdom teeth, or third molars, are commonly referred to oral surgeons, however your general dentist may be more than capable of providing top notch treatment at a lower cost. This will vary significantly from dentist to dentist.
A good first place to start is your current dental home. First off your regular dental office will be able to determine if you actually require oral surgery to begin with. Just as your primary doctor will know which specialty to send you to, your general dentist will know if you need oral surgery and which specialty to send you to. Of course, if you feel more comfortable seeing an oral and maxillofacial surgeon, voice your concerns to your current dental practice and they will refer you to the proper specialty practice. If you don’t have a regular dentist, you can find one through various resources such as the American Dental Association.
How are Oral and Maxillofacial Surgeons Different from Other Surgeons?
Dentists who want to specialize in oral and maxillofacial surgery must first attend dental school and be exceptional within their class. After graduation, these doctors must then attend an accredited oral and maxillofacial surgery residency. Many of these residencies actually require attending the last couple years of medical school in order to obtain their medical degree. Then as medical residents, they shadow and assist a practicing maxillofacial surgeon eventually gaining enough experience to perform the maxillofacial surgery under proper supervision.
What Do Oral Surgeon Residents Learn?
Typically over four years, these oral and maxillofacial surgery residents learn the full scope of advanced care and treat severe cases often in a hospital setting. Many of these surgeries required advanced care and monitoring because the patients are placed under general anesthesia where it is safest to do in a hospital. They gain experience with advanced procedures including corrective jaw surgery, dental implants, advanced bone graft, cleft lip and palate repair, impacted teeth (most often wisdom teeth) extractions, pain and patient management, administration of various types of anesthesia including local, moderate, deep and general anesthesia, sleep apnea and other general surgery training. Additionally, the oral surgeons in training also learn facialThe ‘outside’ surface of the teeth that directly face either the lips or cheeks. reconstruction and even plastic surgery.
In order to be called an oral surgeon, the doctors in training must first meet the requirements of their respective residency program to become board eligible. After passing various testing including their board certification, they may now be called oral surgeons and may decide to practice solely in a dental office or may want to retain their hospital privileges to perform the more advanced surgeries. Even after graduation, the doctors must continue to receive additional continuing education and training and are still held to the standards set by their governing bodies such as the American Association of Dental Boards and the American Association of Oral and Maxillofacial Surgeons (AAOMS).
What Procedures are Considered Oral Surgeries?
Oral surgery encompasses many, many different procedures as previously mentioned. Straightforward gum tissue surgeries such as a maxillary labial frenectomy, a simple tooth extraction procedure and dental implant placement can all be considered oral surgery. While the advanced surgeries are necessary and performed regularly, if you have had oral surgery it was mostly likely one of the more common procedures.
Dental Extractions
Perhaps the most common surgical procedure performed, dental extractions result in thousands of teeth removed across the country every day. These teeth may be removed for various reasons including pain, decay, infection, pathology, or prophylactically as is often the case with wisdom teeth. Depending on the complexity of the oral and maxillofacial surgery, the procedure may be done by your regular dentist depending on his or her skill level.
Your dental home most likely regularly extracts teeth, however if there are increased complexities within the tooth, teeth, bone, or jaw, you may need to see an oral and maxillofacial surgeon. Very often extractions, including wisdom teeth, can be completed in a single appointment and while there will be some post operative pain, the recovery is generally straightforward.

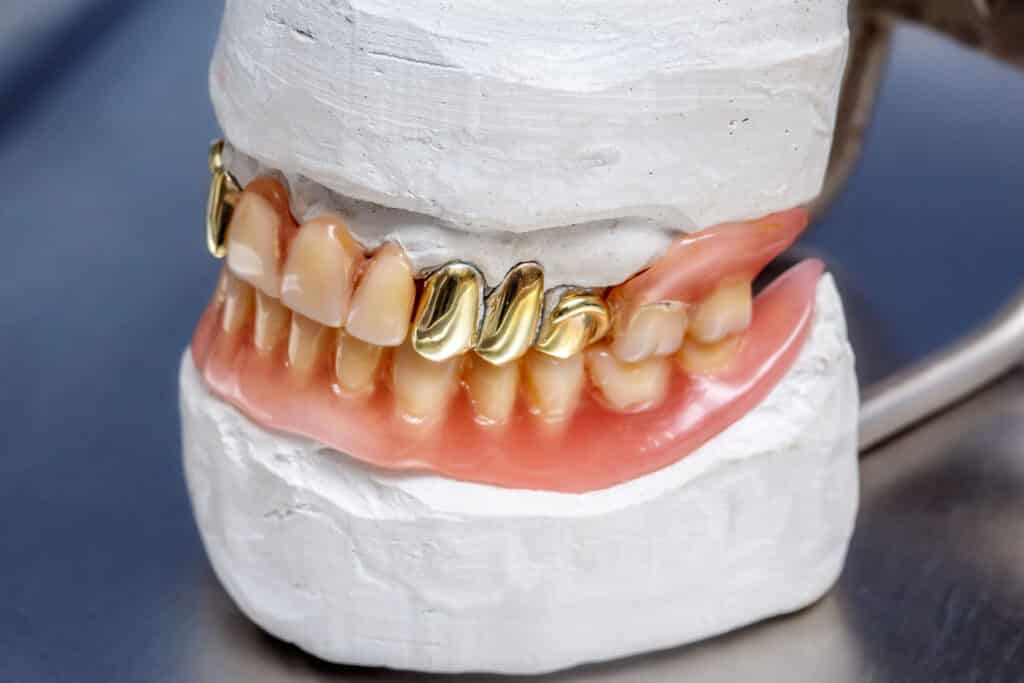
Dental Implants
Whenever a tooth is lost due to various reasons, they will usually need to be replaced to ensure optimal oral health. This is especially true if multiple or front teeth are removed. Dental implants are considered by many to be the gold standard. This is due to how incredibly effective they are at restoring normal function and appearance of extracted teeth. The implants are most often placed directly into the jaws themselves. While they cannot be completed in a single appointment, the end result is as if you get your missing tooth back. There are more limitations and requirements such as adequate bone depth and width, however if you need to replace any missing teeth, implants will often yield the best results.

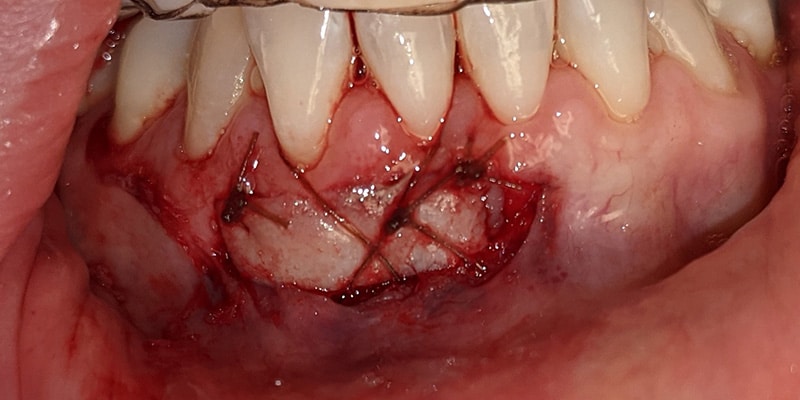
Gum Grafts
As patients age, very often the gums also recede. This specific type of recession is due to a combination of various reasons, including bruxism and heavy brushing but luckily is often reversible. The main goal of various gum grafts is to improve the quality of the tissue in either jaw. This not only improves the long term prognosisThe estimation of how long the proposed treatment will last. of the teeth or dental implant, but also improves esthetics by making the gum line look more natural and even. It is important to understand the quality and height of underlying bone plays an important role in the expectations of the amount of recession that can be reversed using completing soft tissue grafting.
How Should I Prepare for Oral Surgery?
This will depend on the specific procedure performed. Simpler surgeries may not require any preparation, while advanced procedures will require preparation. Ask questions and always listen to your doctors’ instructions as they are in your best interest.
Pre-operation
Most often you will want to wear loose, comfortable clothing and take any medications as instructed. If you are able, you may want to eat a light meal and be hydrated. This may not be possible if you are also receiving IV moderate sedation or deeper as there is the risk of aspirationThe act of drawing a liquid into another vessel or organ. This can occur during administration of local anesthetic if the needle is in a blood vessel. This can also occur if someone vomits water during sedation and inhales the liquid into their lungs., or inhaling, the vomited foods. This may result in death, so it is critical that the instructions are followed.
If a driver is required, ensure transportation is all set and that the driver is easily reached. Your dental office may have additional pre-operative instructions so be sure to ask questions or for additional clarification.
Post-operation
All patients will want to ensure they have adequate time to rest and recover after the surgery. There will be some pain and discomfort while recovering, so avoiding strenuous physical activity is important. If receiving heavier sedation than nitrous oxide, ensure a caretaker will be available for several hours. Take the prescribed or over the counter medications as necessary until the pain is manageable without medication. Eating soft foods for the first few days also helps to avoid complications. The recovery will vary from patient to patient, however with proper time and planning, the post-operative recovery will go smoothly.
What Happens During Oral Surgery?
While the actual steps will vary, the basic process is as follows:
- The procedure is reviewed.
- The patient is sedated (if necessary) and anesthetized.
- The procedure is completed, with most simple procedures in a single appointment.
- The patient then recovers immediately from the procedure, waking up if deeply sedated.
- When appropriate, the patient is dismissed and recovers at home.
What are the Risks of Oral Surgery?
The risks are generally higher with oral and maxillofacial surgery. This is due to the fact that it is a surgery, which inherently carries more risk than non-surgical options.
Minor Risks
- Bruising and swelling
- Pain
- Trismus (painful opening of the jaw)
- Bleeding and blood loss
- Alveolar osteitis (dry socket)
More Serious Risks and Complications
- Infection
- Transient or permanent numbness
- Fractured root tips
- Jaw fractures
- Tooth fragments or other materials pushed into the sinus
- Temporomandibular joint disorder (TMJD)
Be sure you understand the risk to benefit ratio prior to any surgery. Often the benefits outweigh the risks, but even so all patients should understand the potential risks.
What is the Typical Recovery Time?
For most minor to moderate tooth extractions, the recovery varies anywhere from a few days to a couple weeks. More complicated surgeries such as corrective jaw surgery may take a few weeks to a couple months to fully recover. Also the younger and healthier the patient, the faster the recovery time is as well.
How the surgery is performed also plays a role in the post operative pain and recovery time. In short, the more trauma applied to the surgical site will result in more pain and discomfort. When surgical procedures can be completed predictably, the typical recovery time can be shortened.

Does Dental Insurance Cover Surgeries?
Dental insurance covers many oral surgery treatments, but there are many aspects that aren’t covered. Insurance will cover the basics such as the various extractions, however when the plan of action moves further away from bread and butter dentistry and more into surgical medicine, such as removal of an odontogenic keratocyst (OKC) from the jaw, medical insurance may cover the costs.
Sleep apnea is unique in that it can be treated by either a physician with a CPAP machine or a dentist with a mandibular advancement device, but is typically billed through medical. While surgical procedures to treat sleep apnea exist, it is generally agreed that non-surgical options should be explored prior to surgery. If you have any questions regarding billing, find out more information from both your dental home and your insurance.