Humans have a limited ability to regenerate lost body parts and teeth are no exception. Luckily, natural teeth are one of the few body parts that can be replaced that are just as effective in all practical regards as your natural own teeth. While implants are generally the treatment of choice for edentulismMissing some or all teeth in an area of the jaw. or non-restorable teeth, they may not be the best fit for some people. Many situations are unique and require special considerations to ensure if dental implants are truly the right option.
What are Dental Implants?
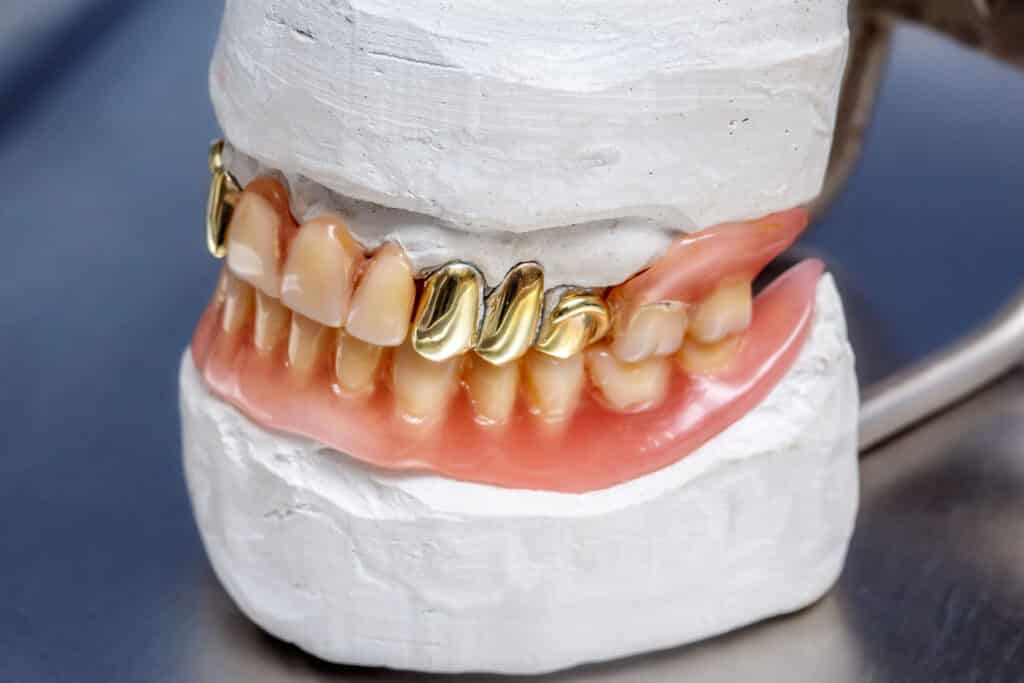
A dental implant is a biocompatible tooth root formThis refers to the shape of implants that mimic natural roots. that fuses to the jawbone via osseointegrationAn intimate, strong, and close connection between living bone and a metal - typically a titanium alloy. With dental implants, it can be generalized as the ‘fusion’ of the implant to the jaw. and acts as a base for an implant supported crown. Dental implants replicate missing natural teeth and very closely mimic the appearance and function of your own teeth. Dental implants also have a very high long term success rate, as shown by many studies1https://www.sciencedirect.com/science/article/pii/S0307904X1000257X2https://web.p.ebscohost.com/abstract3https://www.sciencedirect.com/science/article/abs/pii/S0901502714000976. While there are several types of implants, the most common today are endosteal implantsA type of implant where the entirety of the implant is placed inside of bone with the top of the implant either at the level of bone or gums.. While there are several types of dental implants, the most common today are endosteal implants. Osseointegration is a key process to the success of dental implants, which was described as early as half a century ago by Branemark4Brånemark, P-I., et al. “Intra-osseous anchorage of dental prostheses: I. Experimental studies.” Scandinavian journal of plastic and reconstructive surgery 3.2 (1969): 81-100.. In short, osseointegration is the connection of bone directly to the implant surface5https://www.hindawi.com/journals/bmri/2016/6285620/. The degree of success of an implant is based on the amount of bone loss and the amount and quality of bone to implant contact, where constant research aims to continually improve the already high success rates. Once integrated, the dental implant forms the foundation upon which various oral prosthetics connect to. The most common prosthetic are dental crowns, designed to replace missing teeth due to disease or trauma. Other common prosthetics include implant bridges, removable dentures, hybrid prosthetics and full arch prosthetics. The latter replace conventional dentures for those missing all teeth in either the upper jaw or lower jaw.
Components of a Dental Implant
There are a few key components that make up dental implants. They include the dental implant itself, the implant abutmentOne of the three components in dental implants which connects the implant itself to some type of prosthesis., and the various types of prosthetic teeth. For simplicity sake, we will focus on a single dental implant crown.
- Dental implant – as previously mentioned, this is the root form that is embedded into the maxillaUpper jaw. or mandibleLower jaw.. Implants are made of a medical grade titanium alloyA mixture of metals that aims to blend the best properties of each metal. Gold crowns are not 100% gold, but contain other metals such as platinum, palladium, silver, copper or tin. or zirconia. Zirconia is a biocompatible ceramic with great promise as an alternative material to titanium.
- Abutment – a component that connects the dental implant to the crown. The abutment is what is attached to the implant itself. The connection type plays a large role in the long term implant success due to biological and mechanical properties.
- Dental implant crown – the replacement tooth is visible above the gums that replicates the form and function of the missing teeth. In other words, this is the part that looks like a tooth. The crown itself is retained to the abutment by either cement or a screw.

Requirements for a Dental Implant
There are several requirements for a patient to be clinically eligible for dental implants. First and foremost, the patient must be healthy enough to undergo the dental implant surgery. Not only does the patient need to have a healthy mouth, void of any periodontal disease, but they also should be systematically healthy for the surgical procedure. Uncontrolled health conditions such as diabetes will affect the bone healing phase. Keep in mind implant dentistry as a whole is not black and white but rather a multitude of factors play a role in implant success.
For those healthy enough for maxillofacial implants, the dental implant placement requires sufficient bone to completely encase the dental implant in vital bone. Additionally the dental implants require proper angulation for the placement of the prosthetic teeth. If there isn’t adequate bone, the upper or lower jaw must be augmented. The size range of most dental implants ranges from 3.0mm to 6.0mm in diameter and anywhere from 6mm to 13mm in length, although smaller and larger implants in both dimensions exist.
In addition, there needs to be enough space for the crown itself in the inter-arch and interproximal dimension. Even if there is enough bone, inadequate space to place artificial teeth between your own teeth would defeat the purpose of dental implants. This space can be reduced due to a collapsed vertical dimension of occlusion (VDO) or if the space is occupied by another tooth that has drifted into the edentulous space. If there isn’t enough space for the replacement teeth, the existing teeth must be moved via orthodontics to ensure enough room.
Additionally Risk Factors6https://web.s.ebscohost.com/abstract7https://www.sciencedirect.com/science/article/abs/pii/S0266435611004268:
- Age
- Diabetes
- Smoking
- History of head and neck radiation
- Menopause
- Hormone replacement therapy
- Quality of soft tissues
- Width of implants
- Presence of pathology
There are several studies that have shown that there is not a significant correlation between osteoporosis and early implant failure8https://www.sciencedirect.com/science/article/abs/pii/S09015027173148449http://www.quintpub.com/userhome/omi/omi_8_2_Dao_2.pdf10https://www.ncbi.nlm.nih.gov/. However, treatment for osteoporosis can lead to severe complications such as bisphosphonate related osteonecrosis of the jaw (BRONJ)Exposed, sometimes dead bone, in the jaws that usually occurs after trauma or surgery. The exposed bone is difficult to treat and is a risk for those who have had bisphosphonate treatment for osteoporosis. 11https://www.sciencedirect.com/science/article/abs/pii/S027823911000268512https://journals.lww.com/. The difficulty in implant dentistry is balancing the grafting and prosthetic needs with the risks while placing the largest sized dental implant without damaging the other teeth or structures.
What Are The Pros And Cons Of Dental Implants?
While dental implants are considered the gold standard to treat edentulism, they, like all treatments, are not foolproof and not for everyone. For instance those who are not healthy enough to tolerate the dental implant procedure or who do not want additional surgery may opt to wear dentures instead. There are several other options to replace missing teeth that may be a better treatment option such as fixed partial dentures (bridges) and various removable dentures.
Dental Implant Pros
Implants perform exceedingly well in oral reconstruction and rehabilitation as replacement teeth. The esthetics, occlusion, phoneticsThe study of how humans produce and perceive speech. This is affected by the position of teeth, lip tone, space in the mouth amongst other factors., masticatory ability, and satisfaction rank highly amongst patients13https://onlinelibrary.wiley.com/doi/abs/10.1034/j.1600-0501.2003.140116.x14https://web.p.ebscohost.com/abstract. In other words, they feel and function like real teeth and most patients forget they ever experienced any tooth loss. Dental implants essentially feel like getting your own teeth back.
They are also a versatile treatment option when combining dental implant therapy with various types of prosthesisAn artificial body part, which is often lost due to disease or trauma. such as conventional dentures, resulting in higher patient satisfaction15https://web.p.ebscohost.com/abstract16https://www.researchgate.net/. In addition to excellent function, dental implants also display a high long term success rate ranging from around 85% to as high as 95% over 5 – 10 years in dental research17https://www.sciencedirect.com/science/article/abs/pii/S027823910300726218https://europepmc.org/article/med/2261189919https://www.sciencedirect.com/science/article/abs/pii/S030057121930049120https://link.springer.com/article/10.1007/BF01133326. The evidence points towards dental implants being one the most effective and longest lasting treatment plan option.
Dental Implant Cons
While dental implants have shown to be an extremely effective treatment option, there are several hurdles to pass prior to being a viable treatment plan. Many people are simply not good candidates for a dental implant procedure. The following must be satisfied prior to surgery:
- Healthy surgical candidate
- Sufficient bone depth and width
- Sufficient prosthetic space
- Ability to afford dental implant surgery
The patient must be healthy enough to undergo surgery. The ASA classificationA way to categorize patients in terms of overall health. is a good guideline where ASA class I and II are good surgical candidates as opposed to ASA class III or higher. Unhealthier patients aren’t precluded from surgery, however there are additional risks. The patient should also a healthy mouth, void of periodontal disease and decay. They would also have proper oral hygiene in addition to having regular dental visits.
Dental implants require adequate bone height and depth. If they lack bone in either dimension, they must be able and willing to undergo additional bone growth procedures. When an appropriate amount of bone exists, there must also be adequate space in the edentulous site to place the prosthesis. If there isn’t enough room for an implant crown, the implant itself is useless since the crown cannot be attached to the dental implant. Lastly, the patient must be able to pay for the implant treatment itself, including any necessary grafting. While wiggle room exists with these requirements, there are clear boundaries that cannot be crossed no matter how much the patient or dentist wants to.
What are Dental Implants Made Out of?
The two primary materials used for dental implants are titanium and zirconia. While other materials have been used, titanium has been shown to be a superior material and is the most common material used. More recently zirconia has been showing great promise for those who cannot use titanium.
- Titanium implants: Titanium has evolved to be the material of choice for structural replacements in the human body. While previous materials included stainless steel, gold and cobalt-chromium, titanium has proven to be a superior material of choice. The excellent corrosion resistance in a hostile oral environment, along with the biocompatibility and ability to osseointegrate makes titanium an ideal material for dental implants21https://link.springer.com/article/10.1007/BF0113332622https://journals.lww.comx.
- Zirconia implants: Zirconia, a ceramic, is an alternative material to titanium. Zirconia is commonly used as a dental crown material of choice, but is not as widely used as an implant material. As an alternate material, zirconia has good esthetics in addition to biocompatibility, low affinity for plaque, and good mechanical properties23https://meridian.allenpress.com24https://onlinelibrary.wiley.com/25https://www.sciencedirect.com/science/article/abs/pii/S0928493118320009. It is also a good alternative for those patients who cannot or choose not to use titanium.
What are Dental Implants Used for?
Dental implants are used as the foundation for a myriad of prosthetics. Once osseointegrated, they serve as the anchor for the following treatments:
- Single tooth implants – One of the most common uses for dental implants is to replace a single tooth at a time. This is also more common than the other treatment options as a single person can have multiple single tooth implants over a lifetime. If either the maxilla or mandible is completely edentulous, it does not make sense to place 14 separate individual implant crowns in each jaw when there are other much more effective treatment options.
- Implant supported bridge – This treatment is the same concept of a dental bridge as described in the dental crown except the anchor teeth are dental implants instead of natural teeth. The minimum number of teeth this treatment option replaces is three but it can replace more. However as the number of natural teeth being replaced increases, so do the risks of implant failure due to the Law of BeamsA law that states that as the length of an object increases, it flexes more. For example a piece of wood, let’s say a 2x4, that is 10 feet in length will flex and bend easier than one that is 2 feet in length. In dentistry this principle, along with Ante’s law, is used to determine the length of a dental bridge. and Ante’s LawA law referring to the treatment option of a bridge. It states that the root surface of the teeth being replaced cannot exceed the root surface of the anchor teeth. This is combination with the Law of Beams determines the predictability of the length of a dental bridge..
- Implant supported overdentures – Described in detail on our dentures page, this treatment option is also known as ‘snap-in dentures’. It uses conventional dentures and attaches it to dental implants when restoring an entirely edentulous jaw. By anchoring a removable denture to a solid structure, it solves the primary weakness of removable dentures: lack of stability and retention. Dental implants hold the dentures firmly in place, which is especially problematic on the lower jaw. This treatment option is incredibly effective and greatly increases patient satisfaction26https://www.researchgate.net/profile/Merete-Bakke/27https://web.s.ebscohost.com/abstract.
- Full arch or All on four – This is the best treatment option for a completely edentulous jaw who don’t want to wear dentures. A minimum of four, often more, dental implants are placed directly into the jaw and attached to a prosthesis that resembles a complete denture. There are a few differences between this treatment option and implant overdentures. The material is typically a ceramic, usually zirconia, which has better physical and esthetic properties over traditional dentures which are made out of acrylic. They also don’t cover the palate which can help improve taste and comfort. Additionally, the prosthesis can only be removed by a dentist as it is retained onto dental implants with small screws.
What is the Process of Getting Implants?
When no bone augmentation is needed, the treatment for dental implants is a straightforward process. The actual surgery itself takes anywhere from 15 minutes to a couple hours, depending on the type of dental implant treatment and grafting that is required at the time of dental implant placement. A large portion of the work is completed prior to the surgery during the planning phases. A 3D image of the jaw is taken using cone beam computerized tomography (CBCT) technology. The CBCT scan allows the surgeon to view the jaw in its entirety to see major structures including the bone, nerves, blood vessels, and sinuses. The xray itself has a high degree of accuracy28https://link.springer.com/article/10.1007%2Fs10278-010-9339-9, allowing for accurate planning. Once properly planned and the risk factors have been minimized, the dental implant surgery can proceed.
Dental implants are placed in one of two situations – either in an edentulous site or immediately after a tooth has been extracted. In either situation, the critical principles remain the same. After the patient is comfortable and has been properly numbed with local anesthesia:
- If necessary, the tooth is removed atraumatically.
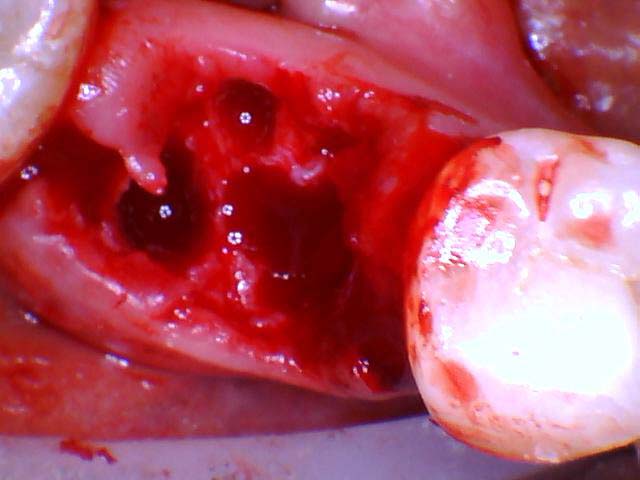
- The jawbone is adequately visualized which may or may not require placing a gingival flap.
- An initial pilot hole is made into the jaw, ensuring proper depth and orientation in 4 directions: mesialThe surface of the tooth that is between teeth and is closest to the midline., distalThe surface of the tooth that is between the teeth and is furthest away from the midline., lingual, buccalThe same surface as ‘facial’ but technically only on posterior teeth..
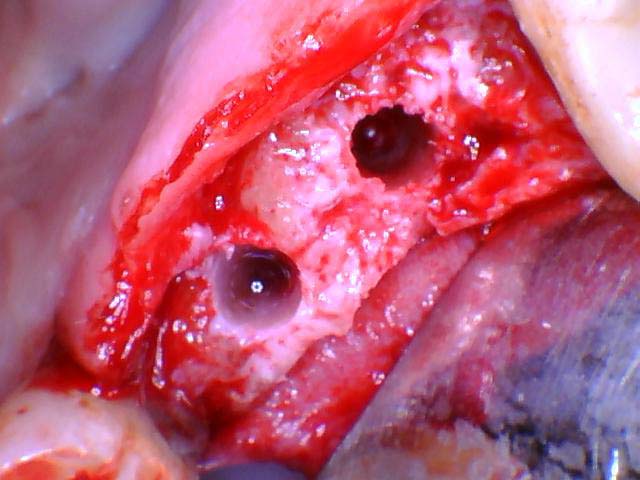
- Subsequently larger drill sizes are used to widen the osteotomy site.
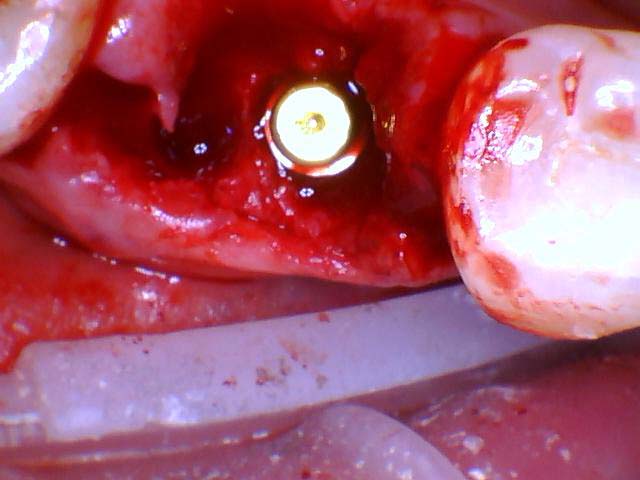
- Once the osteotomy site is an appropriate size, the implant is slowly torqued into place.
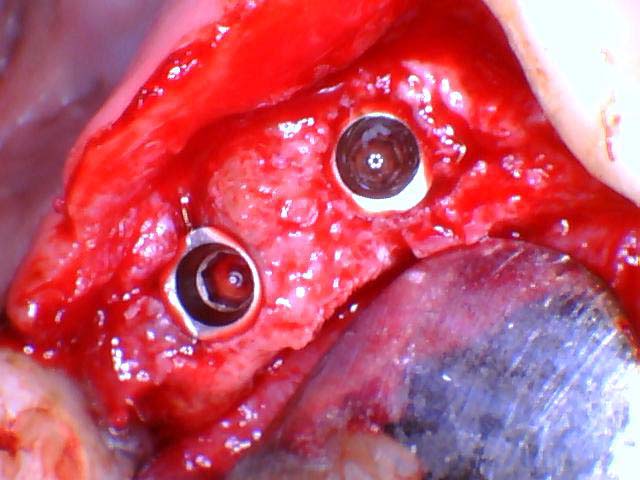
- Depending on the stability of the implant, either a healing cap or cover screw is placed and torqued down.
- If additional grafting at the time of implant placement is needed, it is completed at this time.
- If reflected, the gingival flap is approximated in a tension free manner to prevent the sutures from reopening.
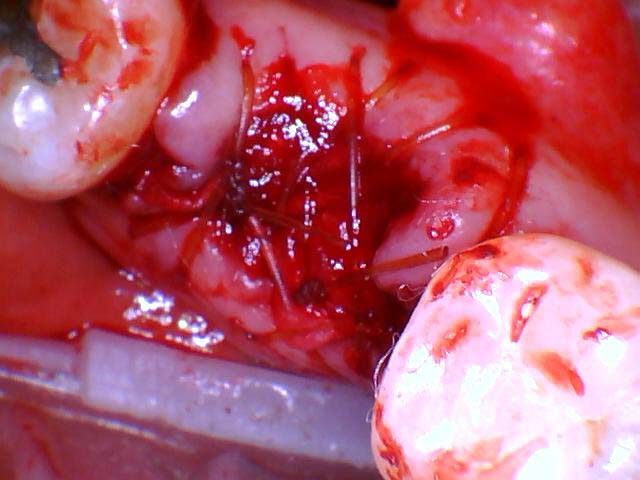
- As the dental implant heals, proper care and good oral hygiene is important to prevent failure. The healing time is most often 3 months. Putting a new tooth immediately after the implant surgery, a procedure called immediate loading, is possible but it carries higher risk. The surrounding bone around the implant may not heal correctly, in which the dental implant surgery would need to be redone.
- Once properly healed, if a healing cap isn’t already present, it is placed during a process called second stage implant uncovering. This very minor procedure done under local anesthesia and is often referred to as the 2 stage implant process. It takes a few weeks for the gingival tissues to recontour and heal.
- A digital or analog impression is taken and sent to the lab to fabricate the abutment and crown.
- Once the implant crown and abutment is made, it is placed onto the dental implant via either a screw or cement. A few important aspects of the crown are checked then the entire process is done! The entire process from dental implant placement to the placement of the permanent artificial teeth can take anywhere from 4 to 12 months.
During the dental implant surgery, copious irrigation (typically saline) is used to prevent overheating the bone. Additionally, throughout the process various radiographs (x-rays) are taken to ensure correct angulation of the osteotomy.
This process is for a single edentulous site and very similar to a multi-tooth edentulous site. However as previously mentioned, there are other uses for dental implants. While the implant placement process is essentially the same, the prosthetic side will vary depending on the type of restorationA synthetic material that replaces either part or the whole tooth that is missing due to disease or trauma. being completed.
What is the Healing Process After Implant Surgery?
As previously mentioned, the healing process typically takes 3 months after surgery for the dental implant to heal and fully integrate. Typically recovery to regular activities takes up to a week or two. It is during this time when it is recommended to eat soft foods and follow the post operative instructions to prevent infection.
How Long do Dental Implants Take?
From the time of the dental implant surgery to the permanent replacement tooth being place typically takes 4-12 months. The process takes longer if the dental implant cannot be placed immediately after extraction. This occurs if the surgeon has reason to believe immediate implant placement will fail, resulting in excessive bone loss. A few of the reasons may include remaining pathology such as a dental infection, poor stability, inadequate blood supply, or a traumatic extraction resulting in fracturing the jaw – most often the buccal plate. If this occurs, it is most predictable to graft the site and wait 3-5 months for healing of the bone.
Once the site has fully healed and adequate bone has been verified via CBCT, the dental implant can be placed, initiating the 3 month waiting prior to loading. A few exceptions to waiting to place a replacement tooth immediately are full arch cases and occasionally anterior implants for esthetic reasons. However there must be 100% patient compliance with immediately loaded implants as any movement will prevent proper healing.
How Much Time do I Need to Take Off After Implant Surgery?
While the recovery time varies on a multitude of factors, typically a patient can return to light duties after a day or two. Typically after a week or so, a patient can return back to regular activities with the exception of strenuous exercise. The following are a few variables that typically increase the recovery time:
- Extraction of a tooth prior to implant placement (immediate implant treatment).
- A more traumatic extraction.
- Complicated health history – (e.g. diabetes).
- Age.
- Multiple dental implants/extractions necessitating a bigger surgery.
- Level of sedation.
- Grafting required at the time of dental implant surgery.
- The patient’s occupation. Someone with a more physically demanding job may need more time off after dental implant surgery. For instance a construction worker may need more time to recover than a desk worker due to the higher required levels of physical exertion.
A good general rule of thumb is the more complicated the surgery, the longer the recovery time will be. The opposite is also true: a single implant placement in an already edentulous site in a healthy ASA I-II patient may return to normal duties (except strenuous exercise) the very next day. If you have any concerns about the recovery time, contact your dental office to get a better idea of how much time you may need.
Other situations to call your dentist are abnormally painful symptoms after treatment. Most often this is after tooth removal. When there is radiating pain that is not manageable with the recommended or prescribed postoperative analgesic medication, you may have a complication that requires medical intervention. In these situations, you should call your dental office to see if these symptoms are abnormal and if additional treatment is necessary.
How Painful are Dental Implants?
Many patients feel anxious prior to dental implant surgery, often believing it to be extremely painful. However the pain experienced following surgery of a single dental implant is typically mild29https://aap.onlinelibrary.wiley.com/doi/abs/10.1902/jop.2007.060032 and can be easily managed with short term NSAID analgesics30https://link.springer.com/article/10.1007/s00784-021-03859-y. However as the number or complexity of dental implants increases, so does the post operative discomfort.
Many patients generally agree that dental extractions are more uncomfortable than a standalone implant surgery. For instance an uncomplicated single implant may rank at a 0-2 on the pain scale whereas a full arch with extractions may be up to a 7-8. These are generalizations as the pain tolerance from patient to patient will vary greatly. If you have any concerns or questions, contact your local dental office.
How Much do Implants Cost?
The cost will vary upon many factors, however depending on the surgery and prosthetic, dental implants can cost anywhere from $3,000 – $8,000+ for a single implant, up to $25,000 – $40,000 for an all on X (full arch) procedure on a single jaw. Keep in mind these estimates have a wide range and your experience will vary. These estimated costs cover the surgery as well as the prosthetic costs. These estimates may or may not cover any grafting, sedation, or extractions that are may be required for implant therapy. Contact your local dental office to find out more information.
Does My Insurance Cover Implants?
Although insurance coverage for dental implants will vary greatly between plans, if they are covered, they are commonly covered at 50-80%. Insurance plans often cover the prosthetic costs (the abutment and implant crown) but they may or may not cover the surgical placement of dental implants.
Other factors to keep in mind are the remaining benefits. If the average single implant costs $5,000 and is covered at 50%, then the insurance should cover $2,500 of the costs and your out of pocket should be $2,500. However if the insurance plan only has $1,000 of total benefits, they will only cover a total of $4,000 even though they cover 50% of the $5,000 on paper. This results in an out of pocket expense of $4,000, not $2,500.
Additionally keep in mind insurance plans may have a missing tooth clause which states that the insurance will not cover any missing teeth prior to that plan. This means if you had a tooth extracted 5 years ago and you started with your current plan 2 years ago, a missing tooth clause means the plan will typically not cover anything to replace that missing tooth.
Lastly, keep in mind that insurance plans may also have a waiting period which states that some services, typically major, will not be covered for a period of time. That time frame is usually 12-24 months, meaning if you start an insurance plan with the intention of utilizing coverage for certain services, you may not be able to do so until as much as 2 years later. It is critical that you understand your own insurance plan so there are no surprises. Contact your insurance if you have any questions.
Frequently Asked Questions
While the actual cost varies from many factors such as locality, grafting, insurance coverage, and treatment by a specialist or general dentist, a single implant typically costs between $3,000 – $8,000.
There are variables that will influence the cost, however a full arch case typically costs anywhere from $20,000 -$40,000 per arch. If you need top and bottom, it will cost twice as much.
Implantation occurs when there is adequate bone and no diseased tissue in or near the implant site.
Implantation bleeding occurs during the actual surgery. However your surgeon will not dismiss you if there is any active bleeding.
Implantation bleeding looks like oozing blood seeping from the implant site. This is typically not an issue due to advanced hemostatic techniques as well as proper suturing.
Bleeding from surgery is controlled prior to being dismissed from the office.
Was this post helpful?
Table of Contents
- What are Dental Implants?
- Components of a Dental Implant
- Requirements for a Dental Implant
- What Are The Pros And Cons Of Dental Implants?
- What are Dental Implants Made Out of?
- What are Dental Implants Used for?
- What is the Process of Getting Implants?
- What is the Healing Process After Implant Surgery?
- How Long do Dental Implants Take?
- How Painful are Dental Implants?
- How Much do Implants Cost?
- Does My Insurance Cover Implants?
- Frequently Asked Questions
References
- 1
- 2
- 3
- 4Brånemark, P-I., et al. “Intra-osseous anchorage of dental prostheses: I. Experimental studies.” Scandinavian journal of plastic and reconstructive surgery 3.2 (1969): 81-100.
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30