The temporomandibular joint (TMJ) is an incredibly complicated joint where dysfunction in the jaw joints can lead to chronic pain, headaches, and discomfort. It can take years, even decades, for someone developing chronic TMD to result in debilitating pain. However it affects millions of people every year. For those affected, the journey to healing can be long and frustrating, usually not because of the treatment, but due to being properly diagnosed. Most people do not realize that TMJ disorders can be identified and treated by a well trained dentist.
When most people refer to temporomandibular disorders (TMD) they often refer to it simply as TMJ. For continuity and ease of understanding, we will refer to any dysfunction or problems within the temporomandibular joints as TMD.
What is TMD?
TMD can refer to a multitude of dysfunctions of the stomatognathic system. In most conversations, it refers to severe pain and discomfort within or near the jaw joint itself. However TMD can also refer to any of the following1https://www.scielo.br/j/dpjo/a/NYb5vMrVyPwWqWVnJnXRm9j2https://pubmed.ncbi.nlm.nih.gov/22838003/3https://pubmed.ncbi.nlm.nih.gov/8179643/4https://pubmed.ncbi.nlm.nih.gov/6578661/5https://pubmed.ncbi.nlm.nih.gov/8496480/:
- Popping
- Jaw clicking
- Grinding
- Jaw locking while open or closed
- Soreness
- Neck and facialThe ‘outside’ surface of the teeth that directly face either the lips or cheeks. pain
- Acute or chronic facial pain
- Jaw limited mouth motions
- Earaches or ear pain
The various noises within the joint may or may not be painful.
When do TMD Symptoms Get Worse?
The TMD pain can manifest while at rest but is often exacerbated by activities that require increased exertion, frequent chewing, or extreme jaw movements. The jaw pain can be mild to severe. Typically it a long time to develop chronic, severe pain, often taking years or decades. However there are events that can speed up the process such as trauma and excessive grinding or bruxism.
The pain originates from either an extracapsular or intracapsular source, meaning that the pain can come from either directly within the joint itself or from the jaw muscles utilized while chewing.
What is the Difference Between TMJ and TMD?
In communications, there is no difference between TMJ and TMD. Most people are referring to the same thing. TMJ stands for ‘temporomandibular joint’, which is where the lower jaw bone, or mandibleLower jaw., meets the skull within glenoid fossa of the temporal bone. TMD stand for ‘temporomandibular dysfunction or disorder’, which is a general term for painful or uncomfortable symptoms within the stomatognathic system. Amongst clinicians, TMD is the most commonly used terminology. There are other names such as temporomandibular joint disorders/dysfunctions (TMJD) and cranio-cervico mandibular disorders (CCMD). Again these names all refer to the same concept.
In short, TMJ actually refers to the actual anatomical joint itself, while TMD refers to the disorders, pain, and problems within or near the joint.
What are Some Causes of TMJ?
There are many things, both chronic and acute, that cause TMJ pain. There are multiple contributing factors that result in TMJ including1-5:
- Internal derangement or dysfunctions within the jaw joint itself
- Overactive, spasming muscles of masticationThe act of chewing.
- Parafunctional habits
- Grinding, clenching, bruxism
- Improper body posture
- Trauma
- OcclusalThe ‘top’ of teeth where chewing occurs on posterior teeth. This surface has pits and grooves. schemes
- Abnormal or underdeveloped growth and development
- Stress
Most often there is not a single cause of TMD, but rather a combination of multiple factors resulting in TMJ disorder. Symptoms also arise once a person’s functional capacity is met and exceeded. In other words, once a person is no longer able to tolerate the accumulated trauma and pathologic factors in their stomatognathic system, pain manifests itself. In addition to pain, headaches, discomfort in the TMJ, and even otalgia (typically inner ear canal pain) commonly are present6https://iccmo.org/Content/Files/iccmo_position_paper016.pdf. There are even instances of headaches pain spreading throughout the head and neck.
An extremely common underlying contributing factor is the underdevelopment of the jaws (Link to RS piece here?). Since the growth and development of the jaws occur at a young age and are often not addressed early enough, many people have jaws that haven’t grown to their full potential. This leads to the upper and lower teeth coming together in a pathologic bite. Luckily, most people are able to tolerate the sequelae of underdeveloped jaws and live their entire lives with little to no TMJ pain.
How do the Jaw Muscles Cause TMD Pain?
When the facial muscles have constant muscle tension, it can lead to myofascial pain. The masseters and temporalis, which are the muscles that control jaw movement, are the main culprits. When the inflamed tissue does not have a chance to relax, these muscles have chronic inflammation, leading to imbalances within the musculoskeletal system. Getting these chewing muscles to relax via various TMJ treatments such as stress management behavior then becomes the goal.
What are the Symptoms of TMD?
By and far the most common TMD symptom is jaw pain near and around the joint, which is just in front of the ear canal. A large study in 2007 evaluated over 4,500 patients with TMJ pain and found the following reported symptoms7https://pubmed.ncbi.nlm.nih.gov/17508632/:
- Pain (96.1%)
- Headaches (79.3%)
- TMJ joint discomfort or dysfunction (75.0%)
- Ear discomfort or dysfunction (82.4%)
Upon examination of the symptomatic patients also revealed:
- Sore pterygoid muscles to palpation (85.1%)
- Sore and tender temporomandibular joint to palpation (62.4%)
While these are the most common symptoms of those who have been diagnosed with TMD, there are other symptoms as well:
- Tinnitus
- Ear pressure
- Neck, back, or shoulder pain
- Abnormal jaw movements including:
- Limited opening
- Deviation or deflection of the jaw to the right or left upon opening
- Irregular movements
- Locking, both open and closed, of the jaw
- Limited range of motion of the head
- Abnormal sounds in the ear upon opening or closing
- Popping, clicking, or grinding sounds in the jaw joints when opening or closing
- Dislocated jaw
- Facial asymmetry
- Muscle hyperactivity, fatigue, or spasms of either the masseters (most common), pterygoids, or temporalis
- Discomfort while eating or gum chewing
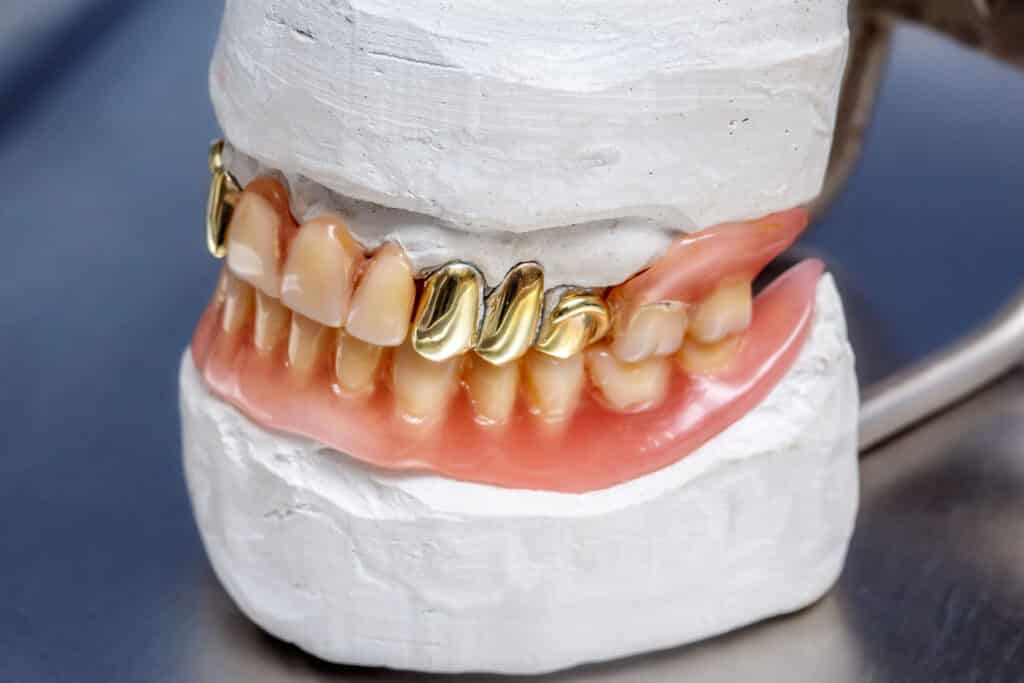
Lastly there are multiple signs and symptoms that may clue in a well trained dentist as to the susceptibility of TMD:
- Abnormal occlusion including crossbites and traumatic occlusion
- Clenching
- Bruxism
- Abnormal wear and tear of the teeth
- Loss of the vertical dimension of occlusion
- Abnormal fracturing of the teeth
- Abnormal movement of upper or lower teeth, including spacing and crowding
- Bite changes
- Bone loss that is not associated with periodontal disease
- Unexplained or frequent root canals, especially if unilateral
- Overall health, including history of rheumatoid arthritis or other degenerative joint disease
Clearly there are a lot of symptoms and clues that can indicate whether or not someone has TMD. Keep in mind that many, many people have one or more of these symptoms without TMD pain. For someone to truly need professional intervention, an thorough exam by a qualified healthcare provider is needed. Once diagnosed, treatment may be rendered to bring the jaw or temporomandibular joint back to health.
How Common is TMD?
It is rather common for people to have some type of dysfunction within the temporomandibular joints itself. While pain is the most common symptom that is the driving factor for treatment, many people can have some type of dysfunction without pain.
These people are able to live with mild or infrequent enough discomfort or are even pain free. These types of TMJ disorders don’t require any type of intervention as they have not exceeded their functional capacity.
Who Makes the Diagnosis for TMJ?
Typically a well trained dentist is the healthcare provider who can make the diagnosis for TMJ disorders. This is not to say that there aren’t others who are able to recognize and help treat temporomandibular disorder. However the ability to recognize TMJ symptoms and treat the root cause often falls to dentists. While dentists’ primary focus are the teeth, gums and jawbones, each jaw joint, the jaw joint disks as well as the airway is also an area of focus amongst specially trained dentists.
What are Some Treatments of TMJ/TMD?
Ultimately the end goal of TMD treatment is the reduction and elimination of pain and return to normal function by bringing the stomatognathic system back into harmony. The treatment will vary depending on the etiologyThe reason why a disease or condition occurs. An example is the etiology of a fractured tooth is from when someone fell down and traumatized the tooth. and can range from relaxation techniques to reduce muscle tension to various surgeries, even jaw joint replacement. Additionally treatment may become multidisciplinary, involving medical specialties such as otolaryngology (ENT), internal medicine, neurology, ophthalmology, rehabilitation, pain management, and chiropractics.
Non-Surgical Treatment for TMJ
As previously mentioned, TMJ pain and dysfunction can be caused by a myriad of sources. However a prevailing school of thought is that the positioning of the upper and lower jaws relative to each other plays an important role. Regardless of orthodontic intervention, everyone has their own habitual or normal bite. An underdeveloped maxillaUpper jaw. will then result in a retruded mandible in order to occlude in that habitual bite. This retrusion then results in an increased and unequal strain amongst the muscles of mastication including the masseters, temporalis, and pterygoids. The primary goal of non-surgical treatment is to re-establish this relationship between the maxilla and mandible to regain homeostasis and harmony.
Medications
Typically the main goal of pain medication in treating temporomandibular disorders is to manage the symptoms in the hopes that the pain will resolve without further intervention. Controlling the pain, inflammation, and hyperactive muscles are the primary goals, thus nonsteroidal anti inflammatory drugs (NSAIDs) and muscle relaxants are often used. For those with severe jaw discomfort, NSAIDs are often not enough to provide adequate pain relief.
Botox
Botulinum toxin, or botox, is another medication aimed to relieve soreness by paralyzing the muscles that control jaw movement. It can also reduce teeth grinding, which can help control pain and relieve stress. However botox is typically used as supplemental treatment to relieve TMD symptoms and must be re-administered at regular intervals.
Physical Therapy
The goal of physical therapy is to retrain the muscles of the head and neck to loosen, relax or strengthen to achieve a better balance when in use.
Massage or Acupuncture
When TMJ symptoms are due to the muscles, massage and acupuncture aims to get the muscles to relax. When the muscles are relaxed, it will relieve pressure off and near the jaw joints which can help relieve pain.
Intraoral Appliances
The primary tool to treat severe TMJ disorders, intraoral appliances refers to the use of an orthotic to reposition the jaws into physiologic rest. When the jaws are repositioned in a manner that allows for minimal muscle activity, fatigue and subsequent pain can be eliminated. Once stable and void of temporomandibular disorders, orthodontic treatment can be rendered to retain physiologic rest.
What Happens When Getting a Dental Orthotic?
A huge advantage of dental orthotics is they are non-invasive and reversible. After diagnosis, the muscles are relaxed using transcutaneous electrical nerve stimulation or a TENS machine. Once the muscles are relaxed enough, impressions are taken in this position called physiologic rest. The orthotic is fabricated to keep the trajectory of the lower jaw in this position to prevent muscle tension and subsequent TMJ disorder pain.
Behavioral Modifications
Minor TMJ disorders can be addressed by changing some habits. When flaring up, one can eat soft foods, avoid extreme jaw movements, and avoid excessive chewing. Avoiding gum chewing and tough chewy foods helps.
Surgical Treatments for TMJ
There are some instances in which severe intracapsular dysfunction results in the necessity of surgical intervention. Often magnetic resonance imaging (MRI) is needed to determine derangement within the joint itself. While some are more invasive than others, they all involve some type of irreversible intervention. A few options include:
Occlusal Adjustment Treatments
This is not surgery in the traditional sense. Instead it is a minimally invasive, but irreversible process. Often called occlusal equilibration, this treatment refers to adjusting the occlusal scheme or in other words how the upper and lower teeth come together. In some instances, this may be able to change the trajectory of a habitual bite. This may work for very minor TMD issues but is often not enough for severe cases of TMD.
Surgery
There are numerous surgeries that involve manipulation of the connective tissue covering the joint or the joint itself. It may involve repositioning the jaw joint disks or mandible itself. A few types of surgeries ranging from arthroscopy to condylotomy.
TMJ Implants or TMJ Replacement
This is a type of total joint replacement that removed the existing joint and replaces it with an artificial joint. This type of surgery is typically reserved for those with severe intracapsular problems.
There is more and more dental and craniofacial research in developing treatment. Of the currently available treatments, many clinicians agree for TMJ treatment, initially starting with non-invasive treatments and titrating up to the most efficacious treatment is the best course of action. This way unnecessary irreversible treatment can be avoided. While there is a time and place for surgeries, many people are happier if resolution can be completed without it.
How Much Does TMJ Treatment Cost?
Since there are numerous surgical and non-surgical treatments that are involved, there is a huge range of costs to treat TMJ pain. Depending on the severity and etiology of pain, it can range anywhere from $5 for some NSAIDs to up to $60,000-$100,000 for total joint replacement surgery. Generally, more invasive surgeries are going to have a higher cost but also may have insurance coverage.
Does Insurance Cover TMJ Treatment?
This will again vary depending on the treatment involved. Over the counter medications won’t have any insurance coverage, however prescription medications may. Non-invasive treatments completed in a dental office may have some coverage, however it will depend on a few factors including:
- In or out of network status
- Covered benefit
- Remaining benefits
Many dental insurances are not progressive enough to include orthotics or splints as part of their covered benefits. Other treatments such as occlusal equilibration and even botox may be covered, however coverage will vary wildly between companies. Speak to your dental office if you have further questions regarding coverage.
Surgical treatments may be different since they are more likely to be billed under medical insurance. Once again the total out of pocket costs will vary depending on a few factors including:
- Covered benefit
- Deductible
- Coinsurance
- Total out of pocket
Since medical insurance may pick up part or all of the cost with the surgical procedures, the initial sticker shock of surgical TMJ treatment should not deter you from receiving proper care.
Was this post helpful?
Table of Contents
- What is TMD?
- What is the Difference Between TMJ and TMD?
- What are Some Causes of TMJ?
- What are the Symptoms of TMD?
- How Common is TMD?
- Who Makes the Diagnosis for TMJ?
- What are Some Treatments of TMJ/TMD?
- What Happens When Getting a Dental Orthotic?
- Behavioral Modifications
- Surgical Treatments for TMJ
- How Much Does TMJ Treatment Cost?
- Does Insurance Cover TMJ Treatment?
References
- 1
- 2
- 3
- 4
- 5
- 6
- 7