An often dreaded procedure, root canals can be associated with fear and viewed as an extremely painful procedure. I have even had some patients who have opted to have a savable tooth extracted over a root canal due to these fears. When done correctly, root canals have mild discomfort and are a proven and critically important procedure that can sometimes give immediate relief to symptoms. We will demystify endodonticsA dental specialty that deals with root canals. These root canals may be completed non-surgically or may require a surgery to complete., also known as root canals.
What is a Root Canal?
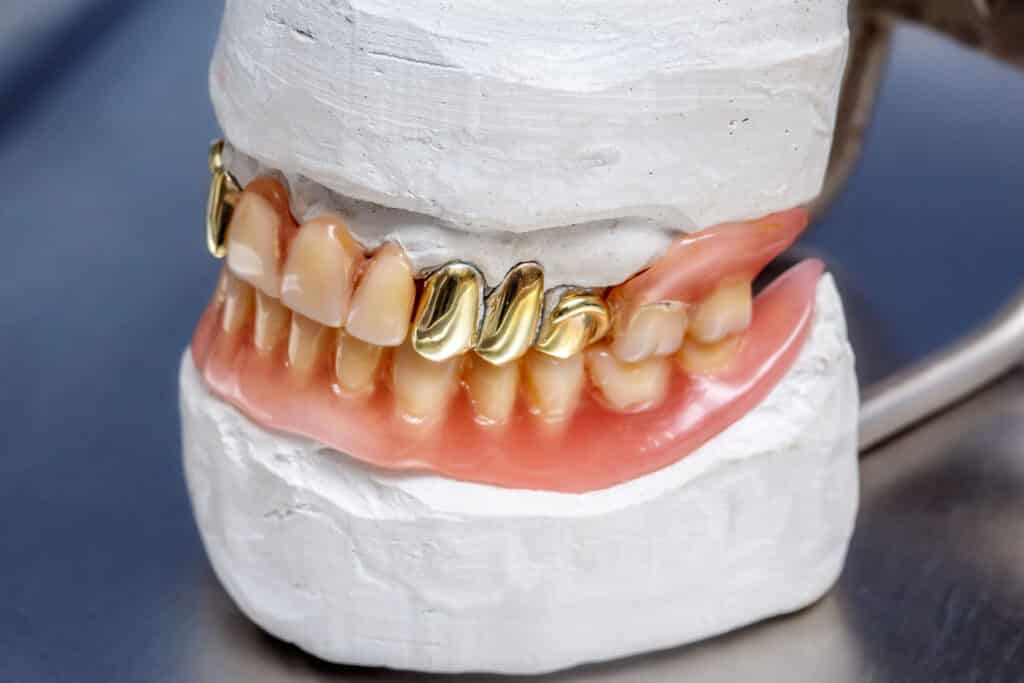
Simply put, non-surgical endodontics treatment is a long skinny filling that replaces the nerve and blood vessels within a tooth. When the pulpThe nerve tissue of the tooth. [nerve] is dying or dead, it eventually leads to an abscess which can be potentially life threatening. The procedure itself is a time consuming and tedious procedure to accurately navigate the canals of a tooth in order to effectively debride and clean. There is also another surgical approach to root canals called an apicoectomy, but is completed less commonly. To understand what a root canal is, we must first understand the anatomy of a tooth.
The Anatomy of a Tooth
A tooth can essentially be broken down to 3 parts: the enamelThe outermost layer of a tooth. Highly mineralized and resistant to decay., dentinThe layer of tooth between the enamel and pulp chamber. and neurovascular bundleA structure that has a combination of two or more of nerves, veins, arteries, and lymphatic vessels traveling in tandem.. The nerves and blood vessels exit the tooth at the apexWhen referring to teeth, it is the very tip of the root where the neurovascular bundle typically exits. through a tiny opening. Every human has roughly the same size, location and anatomy of each respective tooth. Of course there is variability, however a maxillary right first premolar will be similar anatomically across humans. The crown morphology may have small differences, such as the presence or absence of the Cusp of CarabelliA bump or projection on maxillary first molars. It will vary in size, made of enamel and does not need any intervention unless there is decay present.. Where there is more variability is with the root curvature and canal calcification, both of which makes root canals more difficult1https://www.nature.com/articles/ijos201119.
What Causes the Need for Root Canals?
Root canals are needed when there is irreversible pulpitisA condition where the nerve is inflamed and that, as the name implies, is irreversible. When this occurs, the nerve must be removed either by extraction or a root canal. or pulpal necrosis, meaning when the nerve is dying or dead respectively. There will typically be an abscess if necrosis is present as seen in the next figure. The most common cause is tooth decay or cavities, however trauma can also cause it as well.
The enamel, the hardest material in the mammalian body, is resistant to dental decay but not immune. When decay penetrates the outside shell of enamel and reaches the dentin, it will not stop without professional intervention. If left alone, the decay will reach the pulp, cause severe inflammation and eventually kill the nerve. Once dead, the nerve becomes a bacterial breeding ground, eventually exiting through any apices and into the surrounding bone causing an abscess. The abscess can even spread and affect adjacent teeth. Although rare, in the absolute worst case scenario, a dental abscess can cause death. A tooth can essentially be broken down to 3 parts: the enamel, dentin and neurovascular bundle. The nerves and blood vessels exit the tooth at the apex through a tiny opening. Every human has roughly the same size, location and anatomy of each respective tooth. Of course there is variability, however a maxillary right first premolar will be similar anatomically across humans. The crown morphology may have small differences, such as the presence or absence of the Cusp of Carabelli. Where there is more variability is with the root curvature and canal calcification, both of which makes root canals more difficult2https://pubmed.ncbi.nlm.nih.gov/10686905/.
Once present, an abscess will not completely resolve even with antibiotic intervention. In order to get rid of a dental abscess, the source must be removed. This can be done via a dental extraction or a root canal. With a root canal, once the pathologic tissue is removed, the pulp chamberA large space in the dead center of the tooth where a majority of nerve tissue resides. and roots are filled with an inert filling material called gutta perchaA rigid, biologically inert, thermoplastic material that is used to fill canals during a root canal. Its physical properties made it an ideal material to use during root canals. . This is the non-surgical approach of root canals. After the inside of the tooth is cleaned and filled, the body heals and fills in any bony defect over time.
What Happens During a Root Canal?
Similar to restorative dentistry where decayed tissues are removed and replaced with a synthetic material, during a root canal pathologic nerve tissue is removed and filled. Root canals can be a tricky procedure due to the intricacies required to properly find, clean and fill each canal to a very specific length and done without direct vision. An analogy I like to use is endodontics is like being put in a pitch black warehouse, then you need to find the door and pick the lock all in the dark. Although technique sensitive, root canals have saved multitudes of teeth from extraction and are a viable treatment option.
The process is simple, but not always easy:
- After proper sedation and anesthesia, the tooth is isolated from the rest of the mouth using a rubber damA square piece of rubber, typically containing latex, that has a small hole which one or more teeth pass through. It isolates the tooth and acts as a barrier from the rest of the mouth and is used for many dental procedures, especially root canals. There are non-latex versions available for those allergic to latex.. Rubber dams the standard of treatment to prevent bacterial contamination. Bacterial contamination will lead to early failure.
- The pulp chamber is accessed then cleaned and visualized using various burs.
- Once the pulp chamber is opened the canals are located. Depending on the tooth, there are typically 1 to 4 canals. However, it is possible to have 5 or more canals.
- Once the canals are located, they are incrementally widened using endodontic files. During this process, various irrigants are also used to disinfect the canal and dissolve organic matter. This is how the canals are mechanically and chemically cleaned prior to obturationThe filling and sealing of a cleaned and shaped root canal system. In other words, once a tooth’s canal is ready it’s filled with synthetic materials, typically gutta percha and a sealer..
- After the cleaning and preparation of the canals is completed, the gutta percha is fitted and then the canals are obturated using a canal sealer.
- The root canal is now complete and the access is filled with either compositeA synthetic resin that is used for while fillings. This is what most people receive when they get fillings. or amalgam. Depending on the amount of natural tooth remaining, a crown is placed on top of the endodontically treated tooth to increase survival rates
What Pain Can I Expect After a Root Canal?
Depending on the etiologyThe reason why a disease or condition occurs. An example is the etiology of a fractured tooth is from when someone fell down and traumatized the tooth., there can be immediate relief. For cases where irreversible pulpitis is the reason for treatment, immediate relief is often experienced. This is due to the symptoms all arising from an extremely inflamed nerve with infection. Once the pathologic tissue is removed, there is no way to transmit the pain signals to the brain, resulting in immediate relief. I personally experienced this after I had a root canal due to irreversible pulpitis. My tooth was extremely cold sensitive and I tested the tooth postoperatively. Once the anesthetic wore off, I cold tested the tooth and didn’t experience any sensitivity.
The amount of postoperative pain can be less than that pretreatment, especially for those with irreversible pulpitis. For instance if the preoperative pain level is a 9/10 on the pain scale, the pain is usually less, anywhere in the 2-5 range. The postoperative pain can also be managed much better with OTC analgesics. There will always be some amount of soreness due to the length of the appointment and the use of a rubber dam clamp. However that discomfort is generally mild, typically in the 1-3 range and resolves within a few days up to a week.
For those with well pulpal necrosis, the postoperative pain will vary. Typically painful active infections are controlled with antibiotics prior to treatment. Once controlled, the pain level pre and post operative is typically a mild discomfort, in the 1-3 range as previously described. However they are typically not as horrific as many circulating stories describe root canals.
The horror stories circulating about the pain after root canals are the exception to the rule. In the cases of extreme pain, often an adverse event occurred during treatment. One instance is the expression of the irrigants out of the apex of the root of an iatrogenic perforation6https://casereports.bmj.com/content/2015/bcr-2014-207480.short. Rest assured, these are rare events that are not the norm and a vast majority of endodontic procedures occur without incident.
What is a Root Canal Retreatment?
If a previously treated root canal fails, the best option to save the tooth may be to retreat the tooth. A retreatment is simply redoing the root canal by removing the previous gutta percha, recleaning and shaping the root system and refilling with new gutta percha. The most common reason to perform a retreatment is when the first endodontic treatment was poorly done.
This can be an extremely complicated and time consuming procedure. When the tooth is first treated, the root system can be ledgedA term used to describe the creation of a blockage during a root canal. This prevents proper cleaning and shaping of the root system. If this occurs, it does not automatically mean the tooth needs to be extracted. Depending on the location and severity of the ledge, the tooth may not be problematic. or blocked with debris. This makes attaining patency extremely difficult and may not be achievable due to the lack of visualization. The case can still be successful without patency, however it is always best to achieve it. Should a retreatment not be a viable option, another endodontic approach is an apicoectomy.
What is an Apicoectomy?
There is another type of root canal rendered called an apicoectomy. This surgical approach is completed when a non-surgical root canal fails and a new abscess is present. During this procedure, the root tip is visualized after opening a window through the side of the jaw. The pathologic tissue is removed and the defect is thoroughly debrided. Additionally a few millimeters of the root is amputated. The canal is then backfilled then the access is sealed and the abscess resolves. This procedure is completed less frequently than the non-surgical route but is still a viable option to try and save the tooth. However there are cases where even this treatment isn’t viable due to the hopelessThere is no hope to save the tooth and the only viable option is to extract the tooth. prognosisAn estimation of the success and longevity of proposed treatment on a tooth, based on various clinical factors. In other words, how long will the tooth last before needing treatment again. and should have the tooth extracted and replaced with an implant, bridge, or partial denture.
When do I Need a Root Canal?
The most common reason root canals are needed is when trauma or decay negatively affects the nerve. Instances where a patient falls or receives blunt trauma to the teeth can fracture the teeth. If the fracture exposes the nerve, there is very little hope to restore the tooth without a root canal.
More commonly, the dental cariesMost commonly known as a tooth cavity, dental caries refers to decay and rot of the tooth. The breakdown of the enamel and/or dentin is caused by oral bacteria leaving acid on the teeth as a by-product of food consumption. Dental caries is referred to by various names including cavities, tooth rot, and decay. expands and reaches the pulp chamber and causes irreversible pulpitis, eventually leading to pulpal necrosis. The usual progression of pathology goes as follows:
- Decay penetrates the tooth.
- Once decay gets close enough to the nerve, inflammation and sensitivity occurs.
- If left untreated, the inflammation becomes irreversible and severe pain and sensitivity occurs.
- After some time, the nerve dies. At this time, the pain in the tooth goes away which gives the appearance that the problem has been resolved.
- As the nerve dies and bacteria multiplies, a dental abscess forms and begins to affect the jaws and possibly adjacent teeth
- The abscess suddenly ‘blows up’, leading to immense pain, swelling and often emergency dental treatment.
The treatment at each of these stages varies and usually requires more time, complicated procedures and money as the disease progresses.
What are the Symptoms of Needing a Root Canal?
There are a handful of symptoms that indicate a major problem, but pain is the most common. Irreversible pulpitis and a dental abscess, both of which require a root canal, can manifest different symptoms.
Irreversible Pulpitis Symptoms
When the nerve is insulted, resulting in inflammation, there becomes a point when the inflammation will not resolve by itself. Insults can occur from trauma or decay. Even minor dental treatment such as fillings can cause mild trauma to the tooth. The most common symptoms of irreversible pulpitis include:
- Extreme temperature sensitivity, especially to cold. The tooth is more sensitive than usual to temperature fluctuations.
- After temperature sensitivity, the pain lingers much longer than normal. The actual time depends on how long cold sensitivity lasts on healthy teeth. For instance if your teeth are generally very sensitive and any cold sensitivity normally lingers for 8 seconds, an indication of irreversible pulpitis may be sensitivity that lasts 20 seconds. However for most people, lingering sensitivity is typically 5-10 seconds or longer.
- Biting sensitivity. More chewing sensitivity than usual when eating your typical diet may be an indication of a damaged nerve. However biting sensitivity is a symptom of many other problems, such as a cracked tooth.
- A constant chronic dull pain or ache that is exacerbated by any stimulation such as chewing or cold.
These are the most common symptoms of irreversible pulpitis, which is diagnosed based on a combination of these symptoms and a clinical exam. Unfortunately once present, medication is generally ineffective in resolving the condition and resolution necessitates removal of the nerve by a root canal or extraction. While analgesics can help to manage pain, antibiotics are ineffective at reducing pain levels4https://www.sciencedirect.com/science/article/abs/pii/S10792104005443335https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004969.pub4/full.
Dental Abscess Symptoms
Once the nerve dies and the pathology progresses to an abscess, the symptoms and treatment change as well. The most common symptoms include:
- Extraoral swelling and redness. The swelling may occur rapidly and suddenly along with extreme pain. I have had patients say they woke up in the middle of the night with extreme swelling and pain due to an abscess. This swelling can even be seen without looking in the mouth.
- Extreme pain. Similar to irreversible pulpitis, extreme pain is a shared symptom. A key difference is that while the zenith pain levels are similar, a dental abscess can be a constant pain. If the dying nerve in a tooth is stimulated with extreme cold, the pain levels will temporarily spike but they typically subside to a more manageable level. I have had patients tell me that pain from an abscess is constant and more painful than childbirth.
- Intraoral localized swelling. Occasionally there is localized swelling on the gingival tissues near the abscessed tooth that can range in size from a few millimeters to a few centimeters. Depending on the size and extent, the swelling may be incised with the pus and exudate drained.
- Biting sensitivity. Similar to irreversible pulpitis, chewing any food on an abscessed tooth elicits a large amount of pain. A difference is that the tooth may not be cold sensitive. This is due to pulpal necrosis – if the nerve is dead, it cannot transmit any nerve impulses. However there are instances, typically in molars, where part of the nerve is dying while another part of the nerve has necrosed and abscessed. This results in symptoms of both irreversible pulpitis and an abscess.
As the etiology is different, the treatment prior to nerve removal is different. Ultimately the nerve must be addressed by a root canal or extraction, however an abscess is treatable with antibiotics. One or more antibiotics, such as penicillin, amoxicillin, azithromycin, or metronidazole, are used to control the active abscess and reduce the pain and swelling. Often the antibiotics take 24-48 hours to feel noticeable effects and can be managed with analgesics in the meantime. As mentioned previously, sometimes there is a localized swelling on the gingiva that can be drained. If present, draining the abscess can also provide immediate relief until definitive treatment can be rendered.
How Long do Root Canals Last?
Root canals have a high success rate and one can expect an endodontically treated tooth with sufficient cuspal coverage to last 10-15 years7https://downloads.hindawi.com/archive/2011/640509.pdf. There are studies that have shown root canals to last over 20-25 years as well8https://onlinelibrary.wiley.com/doi/abs/10.1111/iej.12908, with the primary reason for failure being fracture.
Personally I have seen endodontically teeth last shorter than the 10-15 year mark, with the shortest lasting only 7 months. Prematurely failed root canals typically failed due to one of two reasons:
- Poor hygiene and lack of regular examinations. This led to non-restorable recurrent decay and subsequent extraction of the tooth as it could not be saved.
- Lack of an appropriate coronal restorationA synthetic material that replaces either part or the whole tooth that is missing due to disease or trauma. (typically a crown). These were on posterior teeth that the patient did not get a crown to protect the tooth. This resulted in early fracture of the tooth that necessitated extraction.
The takeaway is that if you need to get a root canal to save a tooth, practice good hygiene habits and get a crown when necessary to prevent early failure.
How Much Do Root Canals Cost?
The cost will vary depending on many factors, however a good range is $500-$2,000 per tooth. Keep in mind that a buildup and crown may be required in addition to the root canal for longevity. A few factors that influence the cost include:
- Type of tooth requiring treatment. Posterior teeth have more canals and can have more complicated canal systems both of which increase the difficulty of treatment. Root canal prices are typically broken up into one of 3 categories: anterior, bicuspid, and molars with anteriors being more expensive than molars and bicuspids somewhere in between.
- Treatment by a specialist or general practitioner. Specialists usually handle more complicated cases, so they will typically have higher fees.
- Insurance coverage. Dental insurances will typically cover a portion of the fee and can reduce the overall cost if the office is in network with your insurance.
- The type of root canal. Apicoectomies and retreatments are typically more expensive than the standard non-surgical approach.
While expensive, if the tooth can be saved and has a good prognosisThe proposed treatment is the ideal treatment and is expected to last within the usual time frame. For instance if a small piece of tooth is fractured but is easily savable with a crown that is projected to last the expected 10-15 years, the tooth has a good prognosis., it is generally better and cheaper to save a tooth rather than to extract and replace with an implant or bridge.
Frequently Asked Questions About Root Canals
They vary depending on the tooth, number of canals, and experience level of the practitioner, however root canals generally take anywhere from 1-3 hours.
Was this post helpful?
Table of Contents
- What is a Root Canal?
- The Anatomy of a Tooth
- What Causes the Need for Root Canals?
- What Happens During a Root Canal?
- What Pain Can I Expect After a Root Canal?
- What is a Root Canal Retreatment?
- What is an Apicoectomy?
- When do I Need a Root Canal?
- What are the Symptoms of Needing a Root Canal?
- How Long do Root Canals Last?
- How Much Do Root Canals Cost?
- Frequently Asked Questions About Root Canals
References
- 1
- 2
- 6
- 4
- 5
- 7
- 8