Jaw Functional Orthopedics (also known as Functional Jaw Orthopedics) recognizes that, while all humans are fundamentally similar, there’s a significant variance in our builds, impacting our abilities in different tasks. It’s why some humans are tall while others short. These variances result in different body types which affect how that person performs certain tasks. A great example of this is the Olympian Michael Phelps, whose body structure is ideal for competitive swimming.
While some of these variances are affected by genetics, some are impacted by the environment. One of the biggest recent environmental changes we have seen as humans is the shrinking of our mouth and jaws. As the jaws shrank and did not grow to their full potential, the prevailing theory is this has led to many problems. Jaw functional orthopedics aims to correct this by naturally stimulating the neuromuscular system to prevent a multitude of problems.
What is Jaw Functional Orthopedics?
Jaw functional orthopedics is a subset of dentistry that focuses on guiding the natural growth and development of the jaws. By focusing on the stomatognathic system, JFO removes undesirable interferences and stimulates the neuromuscular system during growth and development to guide proper skeletal growth. Many potential problems such as crowding, TMJ issues, and airway problems are addressed and mitigated when the jaws have grown to their full potential.
Some examples of an outside stimulus that affected the growth and development of humans include elongated heads seen in Africa, elongated necks seen in Thailand, and Chinese foot binding. In each of these examples, an outside force is placed on a body part that affects the growth and development of the respective body parts. When done at an early age, the body will conform and grow differently than if no force was applied. This is even seen in deformed turtle shells that got caught in trash.
In these examples, an outside force placed on a growing body resulted in unnatural growth and development. Jaw functional orthopedics aims to essentially to the opposite for ideal growth: add or remove forces which guides the natural and complete growth of the stomatognathic system. It follows the thought that the function determines the shape.
What is the Stomatognathic System?
The stomatognathic system is made up of several parts of the body within the head and neck. These structures include the maxillaUpper jaw. and mandibleLower jaw., the dental arches, multiple muscles including ones used to chew, and the temporomandibular joint (TMJ) to name a few. All these structures work in harmony to do simple tasks such as chewing, swallowing, breathing, and speaking.
Why are Human Jaws Smaller Than Before?
Prior to the industrial revolution, humans had jaws that were simply larger than those of modern humans. Anthropological studies have shown that the discrepancy started to occur as humans shifted from a hunter-gatherer to an agricultural practices1https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0117301. One of the prevailing theories is the type of food that is eaten between the two types of practices is different.
A hunter-gatherer type practice has foodstuffs that are typically harder and requires more effort to grind down. For example dried meats were more common due to lack of refrigeration and root vegetables both require more effort to chew. Flash forward to today’s typical diet which consists of a lot of highly processed and easily chewed foods.
The lack of force and stimulation from chewing softer foods is thought to be one of the primary driving forces leading to smaller jaw sizes. When a young child does not stimulate the jaw enough, they jaws do not grow to their full potential.
Another contributing factor for smaller jaws starts from birth. Breastfeeding requires more force and suction to properly feed as opposed to a bottle. While many babies have an opportunity to breastfeed, many are not breastfed until the ideal age of 18-24 months. Of course, this often is no fault of the parents as societal pressures often do not allow for breastfeeding of that length. As a result, babies are bottle-fed.
The combination of early bottle-feeding and soft foods results in a general lack of stimulation to the jawbones and over the years has resulted in smaller jaw sizes. This has numerous consequences including:
- Crowding and misalignment of teeth
- Smaller airways and nasal passages
- Potential TMJ problems
So Why Doesn’t Everyone Have TMJ, Sleep Apnea, or Crowded Teeth?
While it is true that those who grew up in a post-industrial society often have a smaller jaw size, there are people who can go through their entire lives with minimal to no crowding, no sleeping issues and no TMJ problems. Humans are incredibly adaptive and there are those who have these issues but are able to live a perfectly healthy life. Those who are minimally or not affected and have not met their functional capacity. For example, there are many people who have popping and clicking in their TMJ, a symptom, but who can live their entire life without pain or discomfort.
How Does Jaw Functional Orthopedics Work?
Jaw functional orthopedics uses proprioception and exteroception as stimuli to encourage the musculature to act on the jaws, which directs the growth of the jaws. This is a similar concept to a weightlifter who has higher bone density compared to someone who is physically inactive2/https://ijass.sports.re.kr/, 3https://europepmc.org/article/med/9927006. One theory is the stimulation of the muscles pulling on the underlying skeleton encourages the bone to develop in order to tolerate the increased stimuli. Not unlike someone who works frequently with their hands developing calluses on the palms of their hands.
As it pertains to the jaws, the primary ways that jaw functional orthopedics directs bone growth is through neural excitation. Posture changing and therapeutic posture changing also play a role, however they are essentially a subset of neural excitation.
What is Neural Excitation?
Neural excitation utilizes sensory organs such as the periodontal ligament (PDL), temporomandibular joint (TMJ), and tongue, to send stimuli to the central nervous system and then send information back to the sensory organ. This is to mean that neural excitation is a way for the body to receive various stimulus and react to said stimulus appropriately. When the density of neurons is greater, the body will react differently as opposed to areas of lesser density. As the stomatognathic system contains some of the highest densities of neurons, JFO utilizes this to encourage growth.
An example of this process happens when you eat something unexpectedly hard. Proprioceptors within the periodontal ligament give feedback to the brain about the hardness of food. Eating a soft mango vs hard bread will direct the muscles of masticationThe act of chewing. to generate an appropriate amount of force. If you bite on a rock that’s in your mango salad, in fractions of a second, your jaw will instantly open up. In the way that the stimulus of the rock opened up the jaw quickly, JFO uses neural excitation to stimulate muscles to encourage growth.
What Role do Muscles Play in Jaw Functional Orthopedics?
Muscles are anchored to the underlying bone via tendons and will move the bones when the muscle contracts. This happens anytime a body part is moved. The tongue is ennervated by 5 cranial nerves: the trigeminal, facialThe ‘outside’ surface of the teeth that directly face either the lips or cheeks., glossopharyngeal, vagus, and hypoglossal nerves. Additionally, the tip of the tongue has a high density of sensory neurons. These nerves and neurons act on a number of muscles 8 muscles which make up the tongue.
Four of these tongue muscles, the superior longitudinal, inferior longitudinal, transverse, and vertical muscles are intrinsic muscles which are unique in that they do not insert into bone4https://www.ncbi.nlm.nih.gov/books/NBK507782/. The other four muscles, the genioglossus, styloglossus, hyoglossus, and hyoglossus are extrinsic muscles which insert into one of three bones. The extrinsic muscles attach to the hyoid bone, mandible, or styloid process.
Jaw functional orthopedics takes advantage of the areas of high neural density by stimulating them which then acts on the afrorementioned bones of insertion, with a focus on the mandible. The upper jaws in a very similar way, but via different muscle groups and something called the determinate area.
What is the Determinate Area?
The determinate area refers to a specific positional relationship between the upper and lower central incisors. This position utilizes the high dentistry of proprioceptors within the central incisors. Again by stimulating areas of high neural density, the body growth can be influenced.
How is Jaw Functional Orthopedics Different From Traditional Orthodontics?
Traditional orthodontics focuses primarily on the position of the teeth within the jaws and will sometimes manipulate the jaws via interceptive or stage 1 orthodontics. The first stage of orthodontics manipulates the upper and lower jaws by placing pressure to typically expand the jaws in preparation for braces. This style focuses on the jaws themselves. While there is a shift that incorporates the airway more, jaw functional orthopedics has a more holistic approach.
Jaw functional orthopedics aims to place multiple parts of the body in the correct position in relation to each other. When they are in this optimal position, the teeth will naturally find the correct position, although braces may still be needed for fine-tuning esthetics. These parts of the body include the:
- Temporomandibular joint
- Tongue
- Mandible
- Neck
- Atlantoaxial joint5https://www.ncbi.nlm.nih.gov/books/NBK563271/
- Inframandibular region
- Spine
- Superior air passage
How Does Jaw Functional Orthopedics Change the Jaws?
Jaw functional orthopedics works best when the body is still growing, typically up to the early to mid-teenage range. While it can still work on older adolescents and adults, the growth potential slows down by that age. By identifying the need early, the growth can be influenced and directed as the body grows for optimal results.
Jaw functional orthopedics have a few key concepts used when employing several techniques.
Key concepts:
- Lateral and protrusive movements
- Chewing bilaterally
- Mechanical properties of the consumed foods
- The maxilla and mandible are structurally different and follow different growth and development laws
Jaw Functional Orthopedic Therapy techniques
- Selective grinding
- Direct tracks
- Myofunctional therapy
- Appliances
Key Concepts of Jaw Functional Orthopedics
Lateral And Protrusive Movements
Lateral and protrusive movements are needed to place adequate stimulus to the jaws. The quality of chewing must be good, meaning that the full range of motion needs to occur. Similar to many weight training exercises that focus on complete movements, the full chewing movement allows for better growth and development of the jaws.
Chewing Bilaterally
The act of chewing must occur on both sides and equally. This allows for equal growth, both in volume and height, as opposed to chewing only on one side.
Mechanical Properties of the Foods
The toughness or hardness of the eaten foods should be high. The required amount of force to properly chew a raw carrot is much higher than the force needed to eat macaroni and cheese. Eating whole foods as opposed to processed foods requires more chewing force. By eating whole foods, not only is the child getting better nutrition, but the force placed on the jaws stimulates growth. This concept is similar to that of mewing.
This is thought to be a large driving force of the shift towards smaller mouths. Hunter-gatherer societies do not have the luxury of processed foods. This meant that they either ate whole foods or starved. Fast forward to today, many young children’s foods are processed in a way that doesn’t require heavy chewing. The trick is getting children to actually eat whole foods, which can be difficult to say the least.
Maxilla and Mandibular Growth and Developmental Laws
The growth and development of the jaws will fall into one of 6 categories. These categories are a predictor of the speed and growth potential of the jaws. For instance, there is a category where the speed and growth potential of the mandible is low. While this doesn’t mean this patient cannot be treated, the progress will be slow.
The category will influence the treatment plan and will also set expectations. Each patient is placed into the category via the Petrovic Analysis. The requirements are that the patient must have their permanent maxillary incisors (usually erupting around the age of 6) and must not have had any manipulation to their jaws such as major surgeries or orthodontics.
The Petrovic Analysis helps the doctor to understand the growth trajectories and and implement protocols and set expectations for the best results.
Jaw Functional Orthopedic Techniques
Selective Grinding
This technique analyses the quality of the lateral and protrusive movements. During excursive chewing, an occlusalThe ‘top’ of teeth where chewing occurs on posterior teeth. This surface has pits and grooves. interference may prevent smooth and full lateral movement. In other words, when chewing from side to side, if part of a top tooth sticks out too much, a bottom tooth may run into it which prevents comfortably chewing all the way from one side to another.
By selectively removing the interference, the full range of motion becomes easier. Typically selective grinding is done on baby teeth.
Direct Tracks
Direct tracks is a way to help correct malocclusion. When malocclusion is present, it doesn’t allow for the normal growth and development of the jaws and TMJ. CompositeA synthetic resin that is used for while fillings. This is what most people receive when they get fillings. is bonded onto existing teeth in a way that would re-establish normal mandibular trajectories. By allowing normal lateral and protrusive movements, can bilateral chewing occur as well as encourage normal growth and development.
Myofunctional Therapy
Myofunctional therapy (MFT) can be likened to physical therapy for the tongue. As the tongue plays a huge role in generating stimulus, if the tongue is weak and incorrectly placed, the growth and development potential will be limited. MFT is a way to not only strengthen the tongue, but it also retrains the brain to place the tongue in a better position for not only growth but also may also help with sleeping and breathing disorders as well.
Appliances
Appliances are made to stimulate or inhibit the growth of the jaws. They are able to help guide the growth in transverse as well as vertical problems. For instance a deep bite or an anterior/posterior open bite can all be corrected by using various appliances with different features.
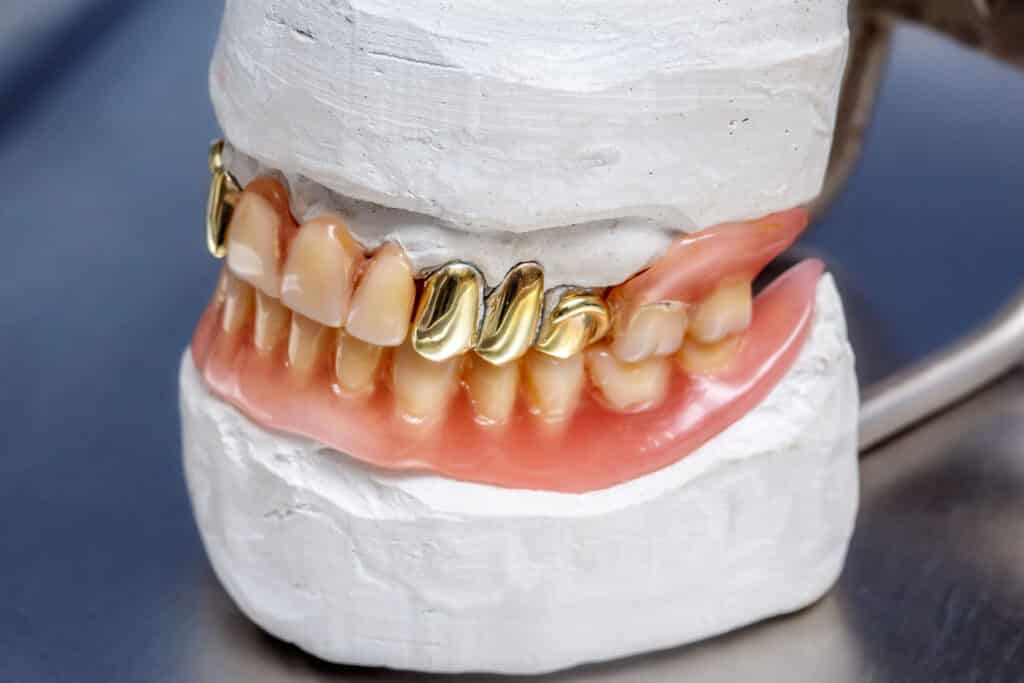
The following slideshow showcases a few different features of Jaw Functional Orthopedic hardware, and how each appliance can vary based on what is being corrected.
What are the Risks of Jaw Functional Orthopedics?
Since JFO is a non surgical, holistic approach, there are few risks that are involved. Some of the primary risks are when growth and development aren’t guided properly. Which happens to be a similar risk to mewing. For example if a patient has a high maxillary growth potential, if the growth isn’t directed properly, the maxilla may grow too much which may necessitate surgical intervention. However this isn’t something that occurs quickly. A well-trained dentist will recognize and prevent this before it becomes an issue.
Is Jaw Functional Orthopedics Right for my Child?
There are many different ways to go about addressing jaw size discrepancies. There are many strategies that address jaw size discrepancies. The premise behind JFO is to naturally guide a growing body to grow to their full potential. This approach looks at the entire stomatognathic system as opposed to other approaches that focus on one aspect within the system.
How Much Does Jaw Functional Orthopedics Cost?
It will vary significantly from practice to practice, however depending on what needs to be done, the cost will range anywhere from $4,000 – $6,500. It can essentially be viewed in the same category as traditional orthodontics and may even have some orthodontic coverage. One practice may include myofunctional therapy while others do not. For more information, speak to your dental office about specific costs.
Table of contents
- What is Jaw Functional Orthopedics?
- What is the Stomatognathic System?
- Why are Human Jaws Smaller Than Before?
- How Does Jaw Functional Orthopedics Work?
- What is Neural Excitation?
- How is Jaw Functional Orthopedics Different From Traditional Orthodontics?
- How Does Jaw Functional Orthopedics Change the Jaws?
- Key Concepts of Jaw Functional Orthopedics
- Jaw Functional Orthopedic Techniques
- What are the Risks of Jaw Functional Orthopedics?
- Is Jaw Functional Orthopedics Right for my Child?
- How Much Does Jaw Functional Orthopedics Cost?
References
- 1
- 2
- 3
- 4
- 5