The gum tissues that covers the bone and fills in between the teeth are a critical part of your oral health. The quality and type of gum tissue plays a large role in prognosisAn estimation of the success and longevity of proposed treatment on a tooth, based on various clinical factors. In other words, how long will the tooth last before needing treatment again. and retention of the teeth. As part of the foundation of the teeth, the gums need to be maintained. Over time, the gums are susceptible to periodontal disease as well as gum recession. When the gums recede, they may require some type of a gum graft to improve the long term survival.
What are Gum Grafts?
A gum graft is a dental surgery in which the quality and/or coverage of the gum tissue adjacent to teeth is improved. Typically this is for receding gums and tooth sensitivity or to improve the quality of thin gums.
While not always done, typically donor tissue is taken from the roof of the mouth and transplanted via various gum grafting techniques to the graft site. The graft tissue is sutured and over time the tissue heals thereby improving the long term survival of the affected teeth.
When Do I Need a Gum Graft?
Gum graft surgery is needed when there is a mucogingival defect and/or significant gum recession. With receding gum tissue, a lack of attached keratinized tissue may be present.
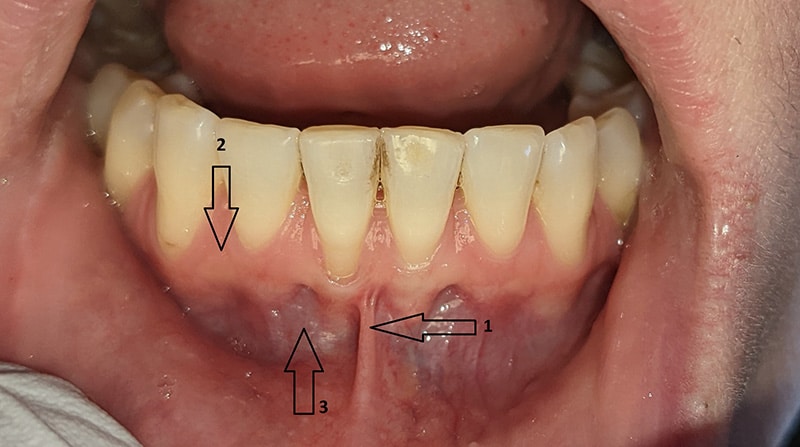
Healthy gum tissue has a thick band of pink, firm tissue which seals out bacteria from invading and causing gum disease. When left untreated, bone and gum tissue continues to recede which leads to eventual tooth loss.
Other scenarios where a gum graft is needed is when there is increased tooth sensitivity, particularly to cold and brushing. When there are exposed tooth root surfaces (the dentinThe layer of tooth between the enamel and pulp chamber.), stimulation to this surface via physical or temperature can cause short, fleeting discomfort. Gum grafting can reverse the recession and eliminate the sensitivity.
Untreated receding gums are at a high risk of extraction over time. In order to prevent dental extractions, a gum graft is recommended to protect the structures surrounding the teeth. Through improving the quality of gum tissue surrounding vulnerable teeth, the foundational gum and bones are less likely to recede over time, resulting in better long term survival rates.
How Prevalent is Gum Recession?
It is estimated that at least half of people have some amount of recession1https://www.sciencedirect.com/science/article/abs/pii/S0002817714619863. Gum recession is very common, however not everyone is a candidate for periodontal surgery. Depending on a few factors including location of the gingival recession, the age of the patient, and the severity of the thinning gums, the patient may or may not need the grafting procedure.
What Causes Gum Recession?
There are a handful of reasons that cause the gums to recede. It is known that it is almost always a multitude of factors, not a single one, that causes gingival recession1https://www.sciencedirect.com/science/article/abs/pii/S0002817714619863,2https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4753713/. The most common reasons include:
- Age. Studies found that older age groups had a very high (70-100%) prevalence of recession1https://www.sciencedirect.com/science/article/abs/pii/S0002817714619863,3https://aap.onlinelibrary.wiley.com/doi/epdf/10.1902/jop.2007.050303. The relationship of age and occurrence of recession is thought to be the longer period of exposure of contributing factors, local and systemic intrinsic changes that come with age and the lesion causing further recession itself.
- Improper toothbrushing. Aggressive, horizontal brushing with medium or hard bristles causes minor lacerations and contusions resulting in detachment and resorption of the bone2https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4753713/,4https://aap.onlinelibrary.wiley.com/doi/abs/10.1902/jop.1994.65.9.864,5https://onlinelibrary.wiley.com/doi/abs/10.1034/j.1600-051X.1999.260502.x. Also brushing with course toothpaste contributes to gum loss.
- Periodontal disease. Poor oral hygiene and plaque buildup leads to gingival recession, in which the lower anterior teeth are especially vulnerable5https://onlinelibrary.wiley.com/doi/abs/10.1034/j.1600-051X.1999.260502.x. Uncontrolled periodontal disease causes bone and gum loss, both which would increase the chances of needed a gum grafting procedure. Additionally, localized inflammation contributes to the breakdown of connective tissue.
- Tooth malposition. When teeth are positioned, either naturally or iatrogenically, not fully set within the jawbone themselves, it contributes to a receding gum line.
- Bruxism. There is a theory that the tiny amounts of flexion of teeth that occurs during heavy grinding contributes towards receding gum tissue.
- Poor habits. Any habit that damages the gum tissues will lead to the need for a gum graft surgery. This can include aggressive use of cleaning tools such as toothpicks or the use of tools not meant for dental cleanings such as a x-acto knife.
Why Do I Need a Gum Graft?
The gingival tissues are a critical part of oral health. The gums cover and protect the underlying bone, which is the foundation of teeth. Having little to no bone to support the teeth is the equivalent of a fence post that is a foot or two deep – neither will last long.
When left untreated, the gingiva will continue to recede which decreases the prognosis of the tooth in a few days. The increased root exposure increases the risk of tooth decay as the exposed dentin is more susceptible to decay. Root caries is especially common amongst the elderly who have more exposed root surfaces. Additionally, the dentin is more prone to plaque buildup which can affect nearby healthy gum tissue.
As the gums recede, the underlying bone also shrinks back as well. When there is less bone surrounding the tooth, it is less stable, which contributes to early tooth loss. Also as gum recession increases, the odds of a mucogingival defect increases as well especially if the gums are already a thin biotype to begin with.
Thick, good quality tissue surround implants is also important for long term success. Implants are also subject to periimplantitis, which is caused from poor quality tissues.

Good oral hygiene helps reduce the need for gum grafting techniques. However even with proper hygiene and professional cleanings, there will still be those who are inherently more susceptible and will need this dental procedure.
What Types of Gum Grafts are There?
When strictly speaking about a gum tissue graft, there are two main types: a free gingival graft (FGG) and a connective tissue graft (CTG). The main purpose of free gingival grafts is to improve the quality of the gingiva. Improving the recession may occur, but is typically not the primary objective. Conversely, connective tissue grafts aim to improve the quality of the gums but more importantly cover the exposed root surfaces.
Free Gingival Grafts
Also called surface grafts, this style of gum graft surgery is relatively straightforward. Sometimes an antibacterial mouthwash is used, then the area of recession is prepared via split thickness flap. If a frenum is present, it is released.
The outside layer of tissue from the roof of the mouth is harvested then transplanted to the surgical site and sutured in place. While typically done under local anesthesia, various types of dental sedation can be administered as well.

It is important that the area not be touched so the donor tissue can form a new blood supply and heal. After the healing process, the existing tissue quality is significantly improved. This slows down further recession and lasts a very long time. However this style of grafting is not preferable in the smile zone due to being unaesthetic.
Connective Tissue Grafts
Also called pedicle grafts, CTGs will feel very similar to to a FGG procedurally. However there are many different ways to perform this gum graft surgery. The pinhole or pinhole-less techniques are two styles that appear to heal much sooner. This is because traditionally, the repositioning of the gingiva requires separating the papilla to some degree.
Depending on the severity of root damage, restorative dentistry may be required prior to surgery. This includes a dental filling or dental crown. Also depending on the severity of the existing recession, complete resolution of the recession may require more than a gingival graft. Advanced bone grafting or other oral surgery may be required for full resolution.
Once again the special mouth rinse may be used, then area of recession is prepared, first with a full thickness mucoperiosteal flap. The root surface is thoroughly debrided and planed if necessary. This cleans the surface to allow for adherence of the pedicle graft tissue. The surface may also be chemically treated to improve chances of success.
The donor connective tissue may be harvested from the roof of your mouth or it may come from a tissue bank. While the tissue from the roof of your mouth is the best due to reduced complications from autogenous grafts, it may not be the best way to perform this gum tissue graft.
The gingiva is the apically repositioned to cover not only the donor tissue, but also the exposed tooth root surfaces and sutured in place. This ensures adequate blood flow to the site, which is critical for success. The surgeon may add a platelet rich fibrin membrane to help aid healing. Once healed, the recession is reversed and it doesn’t even look like a gum tissue graft was done at all.

What Should I Do to Prepare For a Gum Graft?
There is not much to prepare prior to gum grafting. Other than soreness and sensitivity at the donor and recipient sites, gum tissue grafts are not particularly debilitating. That being said, you may want to take a day or two off work especially if your job involves a lot of speaking.
Pre-Operation
Prior to gum graft surgery, any active types of gum disease must first be addressed. Active gum disease may transfer bacteria to the healing site, increasing the odds of a complication. A healthy diet will also help healing. Ensure you understand the gum grafting procedure and be prepared to take some time off work. Ask your dentist how much time you may need to take off.
Post-Operation
With all gum grafting surgery, it is very important that the surgical site not be touched or moved. If the tissue is moved too much, it will impede or interrupt the establishing vasculature. If severe enough, this will cut off blood flow and halt the healing process or even cause unexpected bleeding.
You will want to avoid any physical activity, avoid looking or brushing at the graft site, and eat soft foods for at least a few days. A soft diet may not necessarily mean mashed potatoes and jello, but you will want to avoid extremely hot foods and cold foods. Cool foods that don’t require a lot of chewing are ideal.
Potential Complications
As with all surgeries, gum grafting has a few potential complications. Site soreness, pain, and bleeding are expected. The bleeding will be controlled prior to leaving the procedure room as it is important to achieve homeostasis, especially at the donor site.
A few complications that are more severe are infection, severe swelling, excessive or unexpected bleeding, debilitating pain, paresthesia, and failure of the graft. If you experience any of these, call your dentist for a resolution.

What is The Recovery Time For a Gum Graft?
Usually the recovery time for a gum graft is a few days up to a couple weeks. Although not an inpatient procedure, gum grafting requires modification of activities for a short period of time after surgery. Using tissue from the palate, grafting on multiple teeth, the overall health and any complications will increase the recovery time. The first few days are the most important to ensure minimal activity.
Do I Need to Take Time Off of Work?
It is entirely possible to need to take a day or two off of work. Being prepared to take at least a day off work is prudent, especially if your job requires a lot of speech. While some people can go back to light activities after a day or two, others may take up to a week to return to light activities. Ask your dentist or gum specialist for specifics as each surgery is different.
How Much Do Gum Grafts Cost?
Depending on the type of surgery, the number of teeth, who is performing the surgery, insurance coverage, and locality, the gum tissue graft cost can range from $500 to $2,500 or more. The more complicated and more teeth involved will increase the cost as well as if you need to see a gum specialist such as a periodontist.
Does my Insurance Cover Gum Grafts?
Some dental insurance will cover the procedure while others do not. There are also costs such as added material or techniques such as biologics or platelet rich fibrin that may not be covered. It is difficult to speak to every insurance plan, so speak to your dental office to see how much of the gum graft surgery is covered.
Was this post helpful?
Table of Contents
- What are Gum Grafts?
- When Do I Need a Gum Graft?
- How Prevalent is Gum Recession?
- What Causes Gum Recession?
- Why Do I Need a Gum Graft?
- What Types of Gum Grafts are There?
- What Should I Do to Prepare For a Gum Graft?
- What is The Recovery Time For a Gum Graft?
- How Much Do Gum Grafts Cost?
- Does my Insurance Cover Gum Grafts?
References
- 1
- 2
- 3
- 4
- 5